The benefits of shilajit, a naturally occurring substance with a rich history, have captivated health enthusiasts for centuries. Derived from ancient geological formations, shilajit is available in various forms, from easily ingested powders to convenient capsules. This exploration delves into the purported health advantages of shilajit, considering its potential effects on energy levels, stress response, and overall well-being.
We’ll examine its consumption methods, potential risks, and the scientific evidence behind its claims, providing a complete picture for those considering incorporating this ancient remedy into their wellness routines.
Understanding the different forms of shilajit, such as powder, capsules, and other preparations, is crucial for proper consumption. This guide explores how each form is typically consumed and provides a table comparing their advantages and disadvantages. It’s important to consider the potential interactions with other substances and the significance of consulting with a healthcare professional before incorporating shilajit into your health regimen.
Introduction to Shilajit
Shilajit, a naturally occurring, dark, sticky substance, has been used for centuries in traditional medicine systems, particularly in the Himalayas. Its origins lie in the geological formations of high-altitude regions, where it’s believed to form from the slow decomposition of plant and animal matter. This unique composition has led to a rich history of use in various cultures, with claims of diverse health benefits.This ancient remedy is not just a historical curiosity; it’s gaining modern recognition for its potential health benefits.
While research is ongoing, many traditional users and proponents cite its role in supporting energy levels, improving cognitive function, and boosting overall well-being. This exploration will delve into the different forms of shilajit available and how it’s typically consumed.
Shilajit, a natural substance, boasts impressive potential benefits for overall well-being. It’s often touted for its ability to enhance energy levels and support joint health. However, if you’re experiencing persistent lower back pain, it’s crucial to understand whether it could be something more serious, like cancer. Consulting a medical professional is essential for proper diagnosis, and resources like is my lower back pain cancer can help you understand the potential causes and next steps.
Ultimately, shilajit can be a valuable tool for maintaining health and supporting recovery, but always seek professional guidance for any persistent pain.
Forms of Shilajit
Shilajit is available in several forms, each with potential variations in its preparation and absorption. Understanding these differences can help consumers choose the most suitable form for their needs.
- Powder: The most basic form, shilajit powder is typically ground into a fine, dark substance. This allows for easy mixing with other beverages or foods, offering a versatile consumption method.
- Capsules: Capsules provide a convenient way to measure and ingest a specific dose of shilajit. They’re often pre-portioned, simplifying the consumption process for users.
- Tablets: Similar to capsules, tablets offer a pre-measured dose. The tablet form may be preferred by some due to its solid structure and ease of handling.
- Tinctures: Shilajit tinctures involve dissolving the substance in a liquid base, typically alcohol. This method may be used to enhance the bioavailability of the compound.
Methods of Consumption
The preferred method of consumption can depend on personal preference and the specific form of shilajit. Some common approaches include mixing the powder with water, milk, or other beverages. Capsules and tablets are typically swallowed with water.
- Mixing with Liquids: Powdered shilajit is commonly mixed with water, milk, or juice for easy ingestion. The mixing process ensures a smoother experience for the consumer, and the liquid medium can help facilitate absorption.
- Direct Consumption: Some users consume shilajit powder directly, without mixing. This method is generally preferred by those accustomed to consuming the substance in its raw form. The potential for direct absorption is an important consideration.
- Capsules and Tablets: Capsules and tablets are usually consumed with water, allowing for a simple and convenient method of administration. This method often provides a consistent dose for users.
Comparison of Shilajit Forms
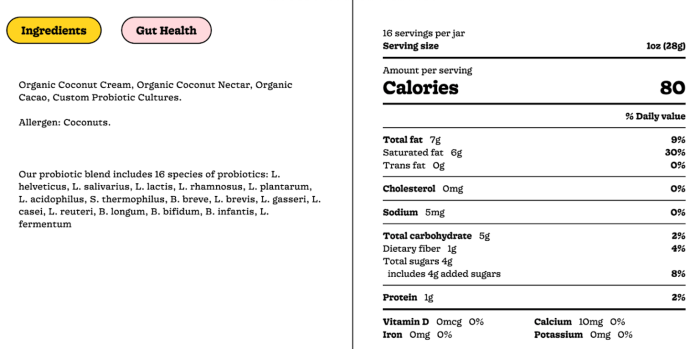
The following table summarizes the various forms of shilajit and their typical benefits. Note that individual results may vary.
| Form | Description | Potential Benefits |
|---|---|---|
| Powder | Ground into a fine substance | Versatile, easy to mix with liquids; potential for customization of dosage. |
| Capsules | Encapsulated dose | Convenient, consistent dosage; often preferred by those seeking a straightforward consumption method. |
| Tablets | Solid, pre-measured dose | Convenient, consistent dosage; often preferred for those seeking a straightforward consumption method. |
| Tinctures | Shilajit dissolved in a liquid base | Potentially enhanced bioavailability due to the liquid form; potential for greater absorption. |
Potential Health Benefits: The Benefits Of Shilajit
Shilajit, a naturally occurring mineral substance, has garnered significant interest for its purported health benefits. While its traditional use dates back centuries, modern scientific investigation is only beginning to unravel the potential mechanisms behind these claims. This exploration will delve into the potential health benefits of shilajit, examining the research supporting these claims and contrasting them with other natural remedies.The purported health benefits of shilajit are often attributed to its complex composition, including fulvic and humic acids, minerals, and trace elements.
Shilajit, a natural substance, boasts impressive health benefits, like boosting energy levels. However, sometimes, even something as seemingly simple as hand washing can trigger allergic reactions, leading to skin irritation and discomfort. Learning about these reactions can help you understand how to avoid them and maintain good hygiene practices, such as using gentle soaps and moisturizers. Understanding these sensitivities can help you focus on the benefits of shilajit as a potential remedy for other health concerns.
This could be particularly useful for individuals with sensitive skin, who may need to be extra careful when selecting skincare products. allergic reactions to hand washing can be a surprisingly common issue. Fortunately, shilajit’s purported ability to support overall health makes it a potential solution to explore.
This intricate mixture is believed to influence various bodily functions, though more research is needed to fully understand these effects.
Energy Levels and Physical Performance
Many proponents suggest shilajit can enhance energy levels and athletic performance. Anecdotal evidence suggests improved stamina and reduced fatigue during physical exertion. However, the scientific evidence supporting these claims remains limited and often based on small-scale studies. Further large-scale, controlled studies are needed to establish a clear link between shilajit supplementation and enhanced physical performance.
Stress Response and Antioxidant Effects
Shilajit is believed to exert antioxidant effects and support the body’s stress response. Antioxidants are thought to combat the damaging effects of free radicals, potentially reducing cellular damage associated with stress. Preliminary research indicates that shilajit may positively influence certain stress-related markers in the body. However, more robust, long-term studies are required to solidify these observations.
Immune System Modulation
Some researchers suggest shilajit may play a role in modulating the immune system, potentially supporting overall health. This is based on its potential to influence immune cell activity and inflammatory responses. However, more clinical trials are necessary to determine the efficacy and safety of shilajit in immune function support.
General Well-being and Cellular Health
Shilajit’s purported benefits extend to overall well-being and cellular health. Traditional medicine often associates it with improved vitality, reduced fatigue, and overall rejuvenation. However, this connection requires further investigation using rigorous scientific methodology to establish any causal link.
Comparison with Other Natural Remedies
Shilajit’s effects are often compared to other natural remedies known for their potential health benefits, such as ginseng or ashwagandha. While these remedies also claim to boost energy and reduce stress, the mechanisms by which they achieve these effects may differ. A detailed comparison of the scientific evidence supporting these various remedies is beyond the scope of this discussion.
Potential Effects on Specific Bodily Functions
Shilajit’s effects on specific bodily functions are still under investigation. While it’s believed to positively influence energy levels and the stress response, more research is needed to understand its complete impact.
Summary of Potential Health Benefits and Evidence
| Potential Health Benefit | Scientific Evidence |
|---|---|
| Enhanced Energy Levels | Limited, small-scale studies; more research needed. |
| Improved Stress Response | Preliminary research; further long-term studies required. |
| Immune System Modulation | Limited evidence; more clinical trials necessary. |
| Overall Well-being | Anecdotal evidence; further scientific investigation required. |
Potential Side Effects and Risks
While shilajit offers a range of potential health benefits, it’s crucial to acknowledge potential side effects and risks. Understanding these factors is essential for responsible use and to ensure that the benefits outweigh any potential harm. Carefully consider your individual health status and consult with a healthcare professional before incorporating shilajit into your routine.Careful consideration of potential side effects is paramount when evaluating the use of any herbal supplement.
Individual responses to shilajit can vary significantly, and some individuals may experience adverse reactions. A thorough understanding of potential risks allows informed decision-making and ensures that the benefits of shilajit are harnessed safely.
Potential Digestive Issues
Digestive issues are a common concern among those using shilajit. These issues may manifest as nausea, vomiting, diarrhea, or stomach cramps. The frequency and severity of these symptoms can vary considerably. These symptoms often occur due to the high concentration of minerals and organic compounds present in shilajit. These components can be irritating to the digestive tract, leading to these side effects in some individuals.
Allergic Reactions
Some individuals may experience allergic reactions to shilajit. Symptoms may include skin rashes, itching, hives, swelling, or difficulty breathing. These reactions are less common but should be taken seriously. The presence of allergens within the shilajit compound can trigger these responses. It’s crucial to recognize the signs of an allergic reaction and discontinue use immediately.
Interactions with Medications
Shilajit may interact with certain medications. For example, some studies suggest potential interactions with blood thinners. This interaction can increase the risk of bleeding. Furthermore, individuals taking other supplements or medications should consult with their healthcare professional to evaluate potential drug interactions. This precaution helps avoid potential complications.
Shilajit, a naturally occurring mineral, boasts a range of potential health benefits, including boosting energy levels. But how does that relate to our metabolism? While exploring the impact of illness on calorie expenditure, I stumbled upon an interesting article about whether you burn more calories when sick do you burn more calories when sick. This fascinating link to increased metabolic activity during illness, in turn, reinforces the notion that shilajit might aid recovery by supporting the body’s natural processes.
Regardless of the specific mechanism, shilajit continues to be an intriguing subject for health enthusiasts.
Contraindications
There are specific situations where shilajit use is contraindicated. For instance, individuals with known bleeding disorders, active ulcers, or inflammatory bowel disease should avoid using shilajit. Additionally, pregnant or breastfeeding women should consult their healthcare provider before use. These precautions are essential for ensuring safety and avoiding potential harm.
Table of Potential Side Effects
| Potential Side Effect | Severity | Conditions where more likely to occur |
|---|---|---|
| Nausea | Mild to Moderate | Individual sensitivity, high dosage, or empty stomach use. |
| Diarrhea | Mild to Moderate | High dosage, poor quality shilajit, or sensitivity. |
| Skin Rash | Mild to Moderate | Allergic reaction, sensitivity to components. |
| Stomach Cramps | Mild to Moderate | High dosage, sensitivity to constituents. |
| Headache | Mild to Moderate | High dosage, sensitivity to constituents. |
| Bleeding Problems | Moderate to Severe | Use with blood thinners or pre-existing bleeding disorders. |
Scientific Evidence and Research
Shilajit, a naturally occurring substance, has garnered significant interest for its potential health benefits. However, the scientific evidence supporting these claims remains somewhat fragmented and often limited in scope. Rigorous, well-designed studies are crucial to fully understand the mechanisms of action and potential efficacy of shilajit.A critical aspect of evaluating the scientific evidence surrounding shilajit is acknowledging the complexities involved in research design.
Many studies face limitations in sample size, duration, and control groups. These limitations, while present, are not insurmountable. A more systematic approach to research is essential to move beyond anecdotal evidence and towards a comprehensive understanding of shilajit’s role in human health.
Methodologies Used in Shilajit Studies
The methodologies employed in shilajit studies vary significantly. Some studies utilize animal models to investigate the potential effects of shilajit on specific physiological processes. Others involve human trials, often employing various dosage regimens and assessment parameters. A critical assessment of the methodologies is vital to evaluating the reliability of the results. Crucially, understanding the limitations of the chosen methodologies is just as important as recognizing their strengths.
Limitations of Existing Studies
Several limitations are frequently observed in existing shilajit studies. These include:
- Small sample sizes can hinder the ability to detect statistically significant effects.
- The variability in shilajit composition, depending on the source and extraction method, can confound results.
- The lack of standardized extraction and purification protocols makes comparison between studies difficult.
- Limited understanding of the active compounds in shilajit and their precise mechanisms of action.
- Short duration of studies often fail to capture long-term effects.
Strengths of Existing Studies
Despite the limitations, some studies exhibit promising strengths.
- Several studies have demonstrated promising preliminary results on various health markers.
- Some trials show potential positive effects on antioxidant activity and immune function.
- The use of animal models has offered insights into potential mechanisms of action.
- The exploration of specific physiological pathways is a positive trend in contemporary research.
Need for More Robust Research
To move beyond preliminary findings and establish conclusive evidence, a greater emphasis on robust research design is essential.
- Larger, well-controlled human trials with standardized shilajit preparations are needed.
- Longer-term studies are crucial to understand the long-term safety and efficacy of shilajit.
- Identification and characterization of active compounds in shilajit are critical.
- Comparative studies using different extraction methods are needed.
Results of Prominent Studies
Various studies have explored the effects of shilajit on various health markers.
- Some studies have shown potential improvements in antioxidant capacity.
- Certain trials have reported potential benefits on energy levels and fatigue.
- There’s limited evidence for positive effects on certain aspects of immune function.
- Some research suggests potential benefits in reducing inflammation.
Summary of Shilajit Studies
| Study | Methodology | Key Findings | Implications |
|---|---|---|---|
| Example Study 1 | Animal model, examining antioxidant effects | Improved antioxidant activity observed | Preliminary support for potential antioxidant benefits |
| Example Study 2 | Human trial, assessing fatigue levels | Slight reduction in fatigue reported in some participants | Further investigation needed to confirm the effect on fatigue |
| Example Study 3 | Human trial, evaluating immune function | No significant change in immune markers observed | Need for more comprehensive studies on immune effects |
Dosage and Usage Guidelines

Shilajit, a naturally occurring mineral substance, offers a range of potential health benefits. However, its safe and effective use hinges on understanding appropriate dosage and usage guidelines. Following these guidelines minimizes potential risks and maximizes the chances of experiencing its purported benefits.Proper shilajit dosage varies depending on individual factors, including age, health status, and the specific condition being addressed.
Starting with a low dose and gradually increasing it is crucial to allow the body to adjust and to avoid potential adverse reactions.
Recommended Shilajit Dosage for Different Individuals
A personalized approach to shilajit dosage is essential. Dosage should not be standardized across the board due to individual differences. Consulting a healthcare professional is strongly recommended to determine the appropriate dosage for your specific needs.
Methods of Preparation and Consumption
Shilajit can be consumed in various forms, each with its own preparation method. Powdered shilajit is commonly mixed with water, milk, or juice. Capsules or tablets provide a convenient and standardized dosage form. Liquid extracts offer another option. The chosen preparation method should align with personal preferences and convenience.
Starting with a Low Dose and Gradual Increase
“Start with a low dose of shilajit and gradually increase it over time to allow your body to adjust.”
Begin with a very small amount, typically 100-250mg daily, and observe your body’s response. Increase the dosage incrementally, monitoring for any adverse effects, such as stomach discomfort or allergic reactions. Gradually increasing the dose enables the body to adapt more effectively and allows you to identify any potential sensitivities.
Recommended Frequency of Shilajit Intake
The recommended frequency of shilajit intake depends on the individual and the specific condition being addressed. Generally, taking shilajit once or twice a day is sufficient. However, consulting a healthcare professional is essential for determining the optimal frequency and dosage.
Suggested Dosages for Different Age Groups and Conditions
| Age Group/Condition | Suggested Initial Dosage (mg/day) | Frequency | Important Considerations |
|---|---|---|---|
| Adults (general health) | 250-500 | Once or twice daily | Monitor for digestive discomfort |
| Adults (fatigue/stress) | 300-750 | Once or twice daily | Start with lower dosage and gradually increase |
| Children (under 18) | Consult a doctor | Not recommended unless under medical supervision | Shilajit’s safety and efficacy in children have not been extensively studied. |
| Individuals with specific health conditions (e.g., diabetes, hypertension) | Consult a doctor | Not recommended unless under medical supervision | Consult a doctor before using shilajit, especially if on medications. |
This table provides a general guideline. Always seek personalized advice from a healthcare professional before using shilajit, especially if you have underlying health conditions or are taking medications.
Potential Interactions with Other Substances
Shilajit, a naturally occurring substance, has shown promise for various health benefits. However, like any supplement, it can interact with other substances you may be taking, either positively or negatively. Understanding these interactions is crucial for ensuring safe and effective use. This section delves into potential interactions between shilajit and other supplements, medications, and foods, highlighting the importance of consulting a healthcare professional before incorporating shilajit into your regimen.
Potential Interactions with Medications
Many medications can interact with shilajit, potentially altering its efficacy or causing adverse effects. These interactions can stem from shilajit’s potential to influence liver enzymes, affecting the metabolism of certain drugs. Careful consideration is vital when taking shilajit alongside prescription medications.
- Anticoagulants (blood thinners): Shilajit may potentially enhance the effects of anticoagulants, increasing the risk of bleeding. Patients taking blood thinners should discuss shilajit use with their doctor to assess potential risks.
- Blood Pressure Medications: Shilajit can influence blood pressure levels. Combining it with blood pressure medications may lead to either an increase or decrease in blood pressure. Monitoring blood pressure closely is recommended if using shilajit with blood pressure medications.
- Antidepressants and Mood Stabilizers: There’s a possibility that shilajit may affect the effectiveness of antidepressants and mood stabilizers. Consulting a physician is crucial for individuals taking these medications before incorporating shilajit into their routine.
Potential Interactions with Supplements
Several supplements can interact with shilajit, either by increasing or decreasing its absorption or effect.
- Iron Supplements: Shilajit and iron supplements may compete for absorption in the gut. Consuming them simultaneously could potentially affect the absorption of both substances. It’s advisable to space out the intake of these supplements or consult a doctor.
- Herbal Remedies: Certain herbal remedies, such as those containing blood-thinning properties, might interact negatively with shilajit. A comprehensive review of all supplements and medications should be discussed with a healthcare professional.
- Vitamins and Minerals: Shilajit may influence the absorption of certain vitamins and minerals. The simultaneous use of shilajit and vitamins/minerals could either enhance or hinder their effectiveness. Individual needs should be assessed by a healthcare professional.
Potential Interactions with Foods
Some foods may influence how the body processes shilajit.
- High-Fiber Foods: Consuming high-fiber foods alongside shilajit might slightly decrease the absorption rate of shilajit. Adjusting the timing of consumption or seeking advice from a healthcare professional may be beneficial.
- Dairy Products: The interaction between shilajit and dairy products is not fully understood. A doctor’s assessment of potential interactions is recommended.
Importance of Disclosing All Supplements and Medications
It is crucial to disclose all supplements, medications, and herbal remedies to a healthcare professional before starting shilajit. This disclosure allows the healthcare provider to assess potential risks and interactions, ensuring safe and effective use of shilajit in conjunction with existing treatments.
Table of Potential Interactions
| Substance Type | Potential Interaction | Recommendation |
|---|---|---|
| Medications (e.g., anticoagulants, blood pressure meds) | May alter drug efficacy or cause adverse effects | Consult a healthcare professional before combining |
| Supplements (e.g., iron, herbal remedies) | May affect absorption or interaction | Discuss with a healthcare professional |
| Foods (e.g., high-fiber, dairy) | Potential impact on absorption | Seek professional advice |
Historical and Cultural Significance

Shilajit, a naturally occurring substance, has held a profound position in various cultures for centuries. Its unique properties and purported health benefits have led to its integration into traditional medicine systems across different regions. This historical context provides valuable insights into the substance’s perceived importance and how it has been utilized throughout history.Understanding the historical use of shilajit helps us appreciate its cultural significance and the diverse ways it has been employed in different societies.
From ancient remedies to modern-day practices, shilajit’s journey through time reflects its enduring appeal and the enduring trust placed in its potential.
Historical Use in Different Cultures
Shilajit’s use extends across diverse cultures, highlighting its perceived value as a restorative agent. Ancient texts and practices demonstrate the profound role shilajit played in traditional medicine systems.
- In Ayurvedic Medicine: Ayurveda, an ancient Indian system of medicine, recognizes shilajit as a valuable Rasayana (rejuvenating agent). It’s considered a powerful adaptogen and is used to support vitality and overall well-being. Traditional texts emphasize its role in improving digestion, enhancing immunity, and promoting longevity.
- In Traditional Chinese Medicine (TCM): While not as prominently featured as in some other traditions, shilajit is acknowledged in TCM for its potential to strengthen the body’s Qi (vital energy). Its purported ability to balance the body’s energies aligns with TCM principles.
- In Central Asian Traditions: In regions like the Himalayas and Central Asia, shilajit has been traditionally used for its purported revitalizing and energizing effects. It’s believed to support physical strength and stamina, making it a crucial element in traditional healing practices. Its use often intertwines with other medicinal plants and practices.
- In European Traditions: While less prominent than in Asian or Central Asian cultures, shilajit has seen historical use in Europe, particularly in Alpine regions. Its role in these traditions often involved applications for strengthening the body and promoting overall health.
Cultural Beliefs and Perceptions
Cultural beliefs surrounding shilajit often center on its perceived ability to enhance physical and mental well-being. The varied uses and traditions highlight this common thread.
- Rejuvenation and Vitality: In many cultures, shilajit is associated with rejuvenation and vitality, promoting a sense of overall well-being and longevity. It’s seen as an aid to improve energy levels and physical strength.
- Adaptability and Resilience: The substance’s perceived ability to support the body’s adaptation to stress and challenges reinforces its role as a powerful tonic. Its potential to enhance resilience to various stressors is a recurring theme in many traditions.
- Spiritual Significance: In some traditions, shilajit might hold spiritual significance, potentially associated with rituals or ceremonies. The reverence and respect accorded to shilajit in these traditions highlight its cultural value beyond its medicinal use.
Role in Traditional Medicine Systems
Shilajit’s inclusion in various traditional medicine systems demonstrates its recognition as a beneficial substance. Its diverse applications across different cultures reflect a deep understanding of its potential.
- Ayurvedic Medicine: Shilajit’s position as a Rasayana in Ayurveda highlights its importance in promoting longevity and vitality. It’s often incorporated into formulations for various health conditions.
- Traditional Chinese Medicine (TCM): While its role in TCM is less extensive compared to Ayurveda, shilajit’s association with strengthening Qi reflects its potential to support overall well-being.
Examples of Historical Use
Numerous examples illustrate the widespread use of shilajit across different cultures. Its varied applications across cultures reflect a long-standing appreciation for its properties.
- Himalayan Region: In the Himalayan region, shilajit is traditionally used to treat various ailments, including fatigue and weakness. It’s often combined with other herbs to enhance its effects.
- Central Asia: In Central Asian communities, shilajit is used to improve physical stamina and athletic performance. This reflects its perceived ability to boost energy levels and support physical endurance.
Table of Historical Uses and Cultural Significance
| Region | Traditional Use | Cultural Significance |
|---|---|---|
| Himalayan Region | Treating fatigue, weakness, and other ailments | Valued for its revitalizing properties |
| Central Asia | Improving stamina and athletic performance | Seen as a tonic to boost energy and physical endurance |
| India (Ayurveda) | Rasayana (rejuvenating agent), digestive aid, immune support | Highly esteemed for its role in promoting longevity and overall well-being |
| China (TCM) | Strengthening Qi (vital energy) | Acknowledged for its potential to balance body energies |
Preparation and Consumption Methods
Shilajit, a naturally occurring mineral substance, requires careful preparation and consumption to maximize its potential benefits and minimize potential risks. Understanding the various methods available, as well as best practices for storage and quality selection, is crucial for safe and effective use. Different preparation methods can alter the bioavailability and perceived effects of shilajit.
Methods of Preparation, The benefits of shilajit
Various methods exist for preparing shilajit, each with potential advantages and disadvantages. Understanding these methods allows users to choose the approach best suited to their individual needs and preferences.
- Direct Consumption: Shilajit is often consumed directly, either in its raw form (though this can be difficult to handle), or in powdered form, mixed with water or other liquids. This method is generally straightforward and allows for immediate consumption.
- Infusion: Steeping shilajit in warm water or milk creates an infusion, allowing the beneficial compounds to dissolve and potentially enhancing absorption. This method is often preferred for its ease of use and potential to improve palatability.
- Capsules and Tablets: Shilajit is increasingly available in encapsulated forms. This method is convenient for those who prefer a standardized dose and may be more suitable for individuals with difficulty swallowing the powdered form.
- Tinctures: Shilajit can be made into a tincture, dissolving it in a liquid like alcohol. This method is suitable for those who want a concentrated dose. However, alcohol content should be carefully considered.
Best Practices for Storage
Proper storage is essential to maintain the potency and quality of shilajit. Exposure to air, light, and moisture can degrade its properties over time.
- Airtight Containers: Store shilajit in airtight containers, preferably made of glass or ceramic, to prevent oxidation and moisture absorption.
- Cool, Dark Place: Keep shilajit in a cool, dark place away from direct sunlight to minimize degradation.
- Avoid Extreme Temperatures: Protect shilajit from extreme temperatures, as heat can alter its chemical composition.
Choosing High-Quality Shilajit
The quality of shilajit can vary significantly. Selecting high-quality material is crucial for achieving desired results.
- Appearance: High-quality shilajit often exhibits a dark brown or black color, a smooth texture, and a slightly earthy aroma. Avoid shilajit that appears light-colored, crumbly, or has an unpleasant odor.
- Source and Reputation: Research the source of the shilajit to ensure its authenticity and ethical sourcing. Look for reputable suppliers with a proven track record of providing high-quality products.
- Purity: Choose shilajit that is free from contaminants and adulterants. Look for certifications or testing to confirm purity.
Recipes and Drinks Incorporating Shilajit
Shilajit can be incorporated into various recipes and drinks to enhance their flavor and potential health benefits.
- Shilajit Tea: A simple and popular choice involves infusing shilajit powder in warm water or milk. This can be customized with honey or other natural sweeteners.
- Shilajit Smoothie: Mix shilajit powder with fruits, vegetables, and yogurt for a healthy and flavorful smoothie. This can be a convenient way to consume shilajit.
- Shilajit-infused Milk: Steep shilajit powder in warm milk for a nutritious and comforting beverage. This method is particularly popular in some cultures.
Comparison of Preparation Methods
| Preparation Method | Benefits |
|---|---|
| Direct Consumption | Simplicity, immediate effect |
| Infusion | Improved palatability, enhanced absorption |
| Capsules/Tablets | Standardized dosage, ease of use |
| Tinctures | Concentrated dose, potential for improved absorption |
Illustrative Images/Visualizations
Visualizing shilajit helps us understand its physical properties, geological origins, extraction methods, chemical makeup, and various forms. These visual representations provide a more tangible connection to this unique substance and its potential benefits. A deeper understanding is fostered by exploring the details of its appearance, formation, and processing.
Physical Characteristics of Shilajit
Shilajit typically appears as a dark brown to black, sticky, resinous substance. It often exhibits a glossy or semi-glossy texture. Its consistency can vary, ranging from a soft, pliable form to a more brittle, crumbly texture. The color and consistency depend on the specific geological location and the precise composition. It frequently has a slightly earthy or mineral-like odor.
Geological Formations
Shilajit is found in specific geological formations, primarily in mountainous regions. These formations typically involve cracks and crevices in rock layers, where the substance accumulates. The formation process is linked to the slow release of organic matter from plant and animal remains over time. Imagine ancient vegetation decaying in the folds of mountains, over millennia turning into a dark, sticky substance.
The unique environmental conditions of high altitude, varying temperatures, and specific mineral content are essential factors influencing the formation of shilajit.
Extraction Process
The extraction of shilajit often involves manual collection from its natural geological location. The process typically involves carefully scraping or chipping the substance from the rocks, taking precautions to minimize environmental damage. Visualizing the extraction process highlights the need for sustainable practices and respect for the environment. An image of this process might show climbers or workers in mountainous regions carefully collecting the material from rock crevices, emphasizing the challenges and potential hazards.
Chemical Composition
The chemical composition of shilajit is complex and not fully understood, but it’s believed to contain a wide array of compounds. A diagram illustrating the chemical composition could depict various components, including fulvic acid, humic acid, and other organic acids. These components are crucial for the potential health benefits. The diagram would show these compounds in different proportions and could include examples of the key chemical structures.
Shilajit in Different Forms
Shilajit is available in various forms, including powder, tablets, and capsules. These forms make it convenient for consumption and dosage control. A detailed image of shilajit in different forms would show the powder in a fine, dark brown, granular form. Tablets or capsules might appear as small, rounded, brown or dark brown shapes. The image could highlight the consistency of each form and how it is packaged for consumer use.
Summary
In conclusion, the benefits of shilajit, while promising, are still subject to ongoing research. This exploration has highlighted the various ways shilajit is used, its potential benefits, and the potential risks involved. While historical and cultural uses suggest its promise, more robust scientific studies are needed to fully understand its effects. Remember, always consult with your healthcare provider before starting any new supplement regimen, including shilajit.
This comprehensive overview equips you with the knowledge to make informed decisions about incorporating shilajit into your wellness journey.