IBS pain or trapped gas can be a frustrating and debilitating experience. This comprehensive guide delves into the complexities of understanding, identifying, and differentiating between these two common digestive issues. We’ll explore the underlying causes, potential triggers, and effective management strategies, helping you navigate this often confusing territory.
From the physiological processes behind gas formation to the subtle yet significant differences in pain characteristics, this article provides a detailed and informative overview. We’ll also examine the role of diet, lifestyle, and underlying medical conditions in both IBS pain and trapped gas, ultimately empowering you with the knowledge to take control of your well-being.
Understanding IBS Pain
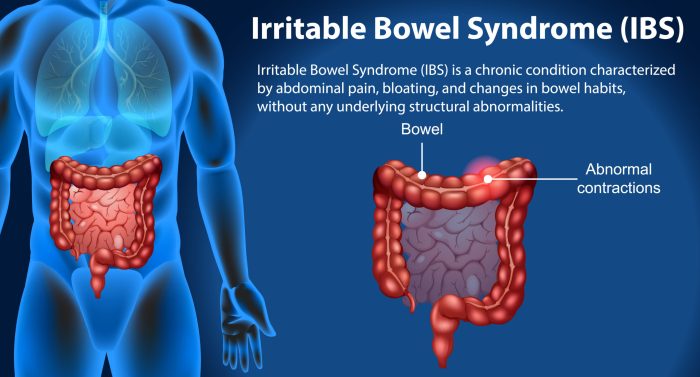
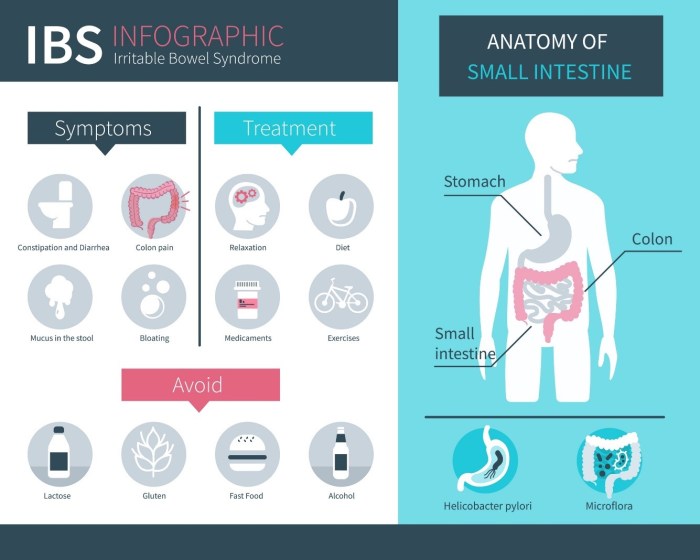
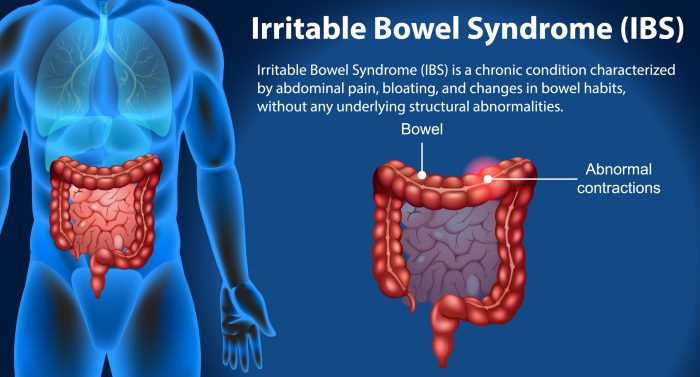
Irritable bowel syndrome (IBS) is a common chronic gastrointestinal disorder affecting millions worldwide. Characterized by recurring abdominal pain, altered bowel habits, and associated symptoms, IBS can significantly impact a person’s quality of life. While the exact cause of IBS remains unknown, various factors contribute to its development and manifestation. Understanding the different types, triggers, and management strategies is crucial for effective self-care and seeking appropriate medical advice.
Irritable Bowel Syndrome (IBS) Overview
IBS is a functional gastrointestinal disorder, meaning there’s no structural damage to the digestive tract. Instead, it involves abnormal muscle contractions and heightened sensitivity in the gut. This leads to symptoms like cramping, bloating, and changes in bowel movements. IBS is often categorized into different subtypes based on the predominant bowel habits.
Dealing with IBS pain or trapped gas can be tough, especially for little ones. Sometimes, similar discomfort can stem from earwax buildup, which can be easily prevented and treated, like in the case of excessive pediatric earwax. Learning how to manage this issue is crucial for overall comfort, and you can find helpful tips on how to prevent and treat excessive pediatric earwax here.
Ultimately, understanding the underlying causes of these issues is key to finding lasting relief, whether it’s gas pain or other discomfort.
Types of IBS and Symptoms
IBS is typically categorized into three main types: IBS with constipation (IBS-C), IBS with diarrhea (IBS-D), and IBS with mixed bowel habits (IBS-M).
- IBS-C: This type is characterized by infrequent bowel movements that are typically hard and difficult to pass. Straining during bowel movements is common, often accompanied by abdominal discomfort and bloating.
- IBS-D: Individuals with IBS-D experience frequent, loose, and watery bowel movements. These episodes can be unpredictable and lead to urgency and discomfort.
- IBS-M: This type exhibits a mix of both constipation and diarrhea symptoms. Patients may experience alternating periods of loose and hard stools, along with varying degrees of abdominal pain.
Comparing IBS Pain with Other Abdominal Pain Causes
Differentiating IBS pain from other abdominal pain conditions is crucial for appropriate diagnosis and treatment. While IBS pain is typically characterized by cramping and discomfort, other conditions like appendicitis, inflammatory bowel disease (IBD), or gallstones can also cause abdominal pain. The location, duration, and intensity of pain, along with accompanying symptoms, can help distinguish IBS from other conditions.
A doctor can evaluate these factors to reach an accurate diagnosis.
Common Triggers for IBS Pain Episodes
Various factors can trigger IBS pain episodes. Diet plays a significant role, with certain foods and drinks acting as triggers for some individuals. Stress, anxiety, and hormonal fluctuations are also frequently identified triggers. Changes in routine or environmental factors can also contribute to IBS symptom flares.
The Role of Diet in IBS Pain Management
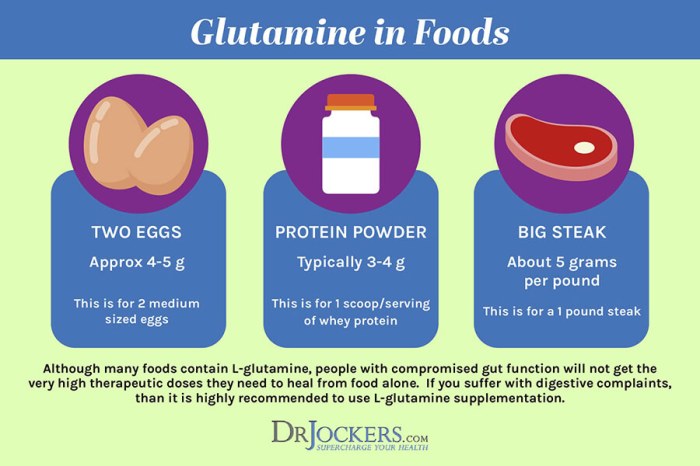
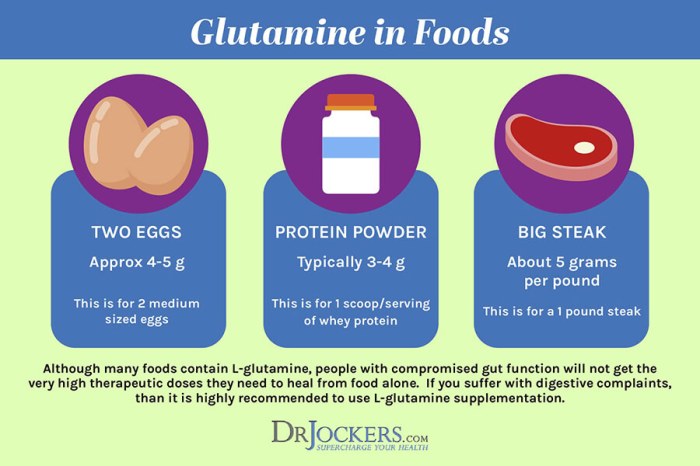
Dietary modifications are often integral to managing IBS symptoms. Identifying trigger foods is crucial. Common triggers include high-fat foods, caffeine, alcohol, certain fruits, and vegetables. A low-FODMAP diet (low in fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) is a common dietary approach for IBS management. It involves reducing the intake of these fermentable carbohydrates that some individuals find challenging to digest.
Consulting a registered dietitian can be beneficial in developing a personalized dietary plan for IBS.
Symptoms of IBS: A Summary Table
| Symptom | Description | Severity | Frequency |
|---|---|---|---|
| Abdominal Pain | Cramping, aching, or throbbing pain in the abdomen. | Mild to severe | Occasional to frequent |
| Bloating | Feeling of fullness or distension in the abdomen. | Mild to moderate | Occasional to persistent |
| Changes in Bowel Habits | Alterations in frequency, consistency, or ease of bowel movements. | Mild to severe | Occasional to frequent |
| Gas | Increased production or difficulty passing gas. | Mild to severe | Occasional to frequent |
Identifying Trapped Gas
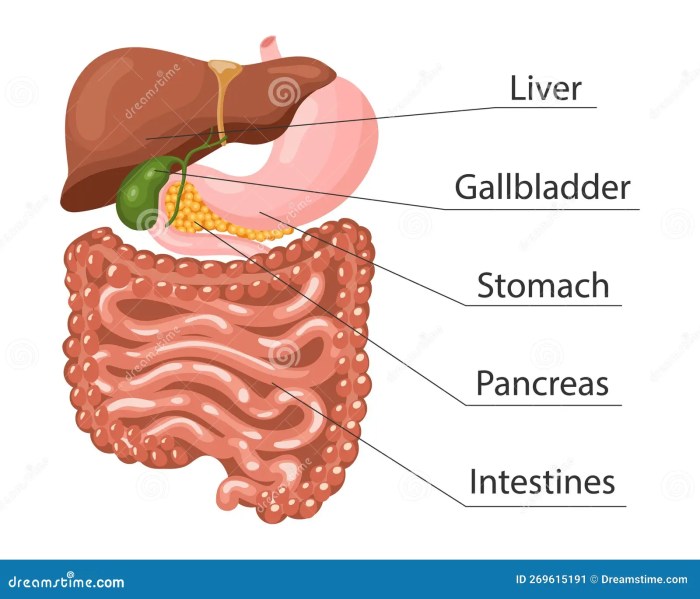
Understanding the difference between IBS pain and trapped gas is crucial for effective management. Often, the symptoms overlap, making diagnosis challenging. This section delves into the physiological processes behind gas formation, the contributing factors, and the key distinctions between the two conditions.The digestive system is a complex network responsible for breaking down food into absorbable nutrients. A byproduct of this process is gas, produced both by the bacteria residing in the gut and by the fermentation of certain foods.
This gas, naturally produced and often harmless, can become problematic when trapped within the digestive tract.
Physiological Processes of Gas Formation, Ibs pain or trapped gas
The human digestive system harbors trillions of bacteria that play a crucial role in breaking down complex carbohydrates. These bacteria produce gas as a byproduct of their metabolic activity. Certain foods, particularly those high in fiber or certain sugars, are more readily fermented by these bacteria, leading to increased gas production. This fermentation process occurs primarily in the large intestine.
The resulting gas can then accumulate, potentially causing discomfort and bloating.
Factors Contributing to Trapped Gas
Several factors can contribute to the accumulation and trapping of gas in the digestive system. Diet plays a significant role, with certain foods being more likely to cause gas. Lifestyle choices, such as chewing gum excessively or consuming carbonated beverages, can also contribute. Underlying medical conditions, such as irritable bowel syndrome (IBS) or lactose intolerance, can exacerbate gas formation.
Foods that Produce Gas
Many foods contribute to gas production. Common culprits include beans, lentils, broccoli, cabbage, cauliflower, onions, and garlic. These foods are rich in complex carbohydrates that are difficult for the body to digest, leading to increased fermentation and gas production. Dairy products, particularly those containing lactose, can also cause gas in individuals with lactose intolerance. Carbonated beverages and artificial sweeteners can also contribute to gas buildup.
Sensations of IBS Pain vs. Trapped Gas
While both IBS pain and trapped gas can manifest as abdominal discomfort, the sensations and characteristics differ. IBS pain is often described as cramping, intermittent, and associated with changes in bowel habits. Trapped gas, on the other hand, is typically characterized by a feeling of fullness, bloating, and pressure in the abdomen. The pain associated with trapped gas is often more localized and intermittent, unlike the often more diffuse and constant pain of IBS.
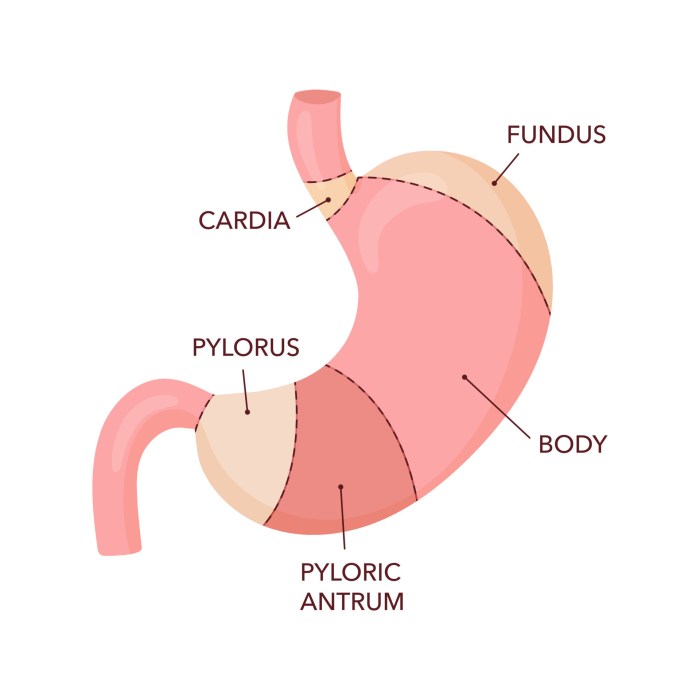
Pain Location and Characteristics
The location of pain can also help differentiate the two conditions. IBS pain can be felt anywhere in the abdomen, often migrating or fluctuating. Trapped gas, however, tends to be more localized to the area where the gas is accumulating, often in the mid-abdomen or lower abdomen. The duration and intensity of the pain also vary.
Comparison of Symptoms
| Symptom | IBS Pain | Trapped Gas | Possible Causes |
|---|---|---|---|
| Pain Location | Variable, often migrating | Localized, often mid or lower abdomen | IBS, muscle spasms, inflammation |
| Pain Character | Cramping, intermittent, potentially severe | Fullness, pressure, bloating | Fermentable foods, air swallowing, medical conditions |
| Bowel Habits | Changes in frequency, consistency, or urgency | Usually no change in bowel habits | IBS, diet |
| Accompanying Symptoms | Nausea, bloating, fatigue | Bloating, belching, discomfort | IBS, diet, stress |
Differentiating IBS Pain from Trapped Gas: Ibs Pain Or Trapped Gas
Pinpointing the exact cause of digestive discomfort can be tricky, especially when symptoms overlap. Understanding the subtle distinctions between irritable bowel syndrome (IBS) pain and trapped gas is crucial for accurate diagnosis and effective management. This often requires careful consideration of various factors, including symptom duration, intensity, and accompanying characteristics.Identifying the precise source of abdominal distress is a diagnostic challenge, particularly when symptoms of IBS pain and trapped gas share some similarities.
The key lies in recognizing the nuances in their presentation. Different individuals experience these conditions differently, and the specific characteristics can help differentiate them.
Diagnostic Challenges in Distinguishing IBS Pain from Trapped Gas
Distinguishing between IBS pain and trapped gas can be challenging due to overlapping symptoms. Both conditions can cause abdominal discomfort, bloating, and changes in bowel habits. The absence of definitive physical findings and the variability of symptoms in each individual make a definitive diagnosis sometimes difficult. This complexity necessitates a comprehensive approach to assessment.
Key Characteristics for Differentiating IBS Pain and Trapped Gas
Several key characteristics can help differentiate IBS pain from trapped gas. Consider the duration of symptoms. Trapped gas discomfort typically resolves quickly, often within a few hours, whereas IBS pain can persist for days or even weeks. The intensity of the pain also plays a role. Trapped gas pain is usually milder and more intermittent than the often intense, cramping pain associated with IBS.
Accompanying symptoms, such as bloating, diarrhea, or constipation, can also aid in differentiation. IBS is often accompanied by these additional symptoms, whereas trapped gas is more isolated to the abdominal discomfort.
Role of Medical History and Physical Examination
A detailed medical history is crucial in differentiating the two conditions. A thorough questioning about the duration, frequency, and intensity of symptoms, along with associated symptoms, helps to identify patterns. A physical examination, including palpation of the abdomen, can sometimes reveal signs of inflammation or tenderness in IBS but not necessarily in trapped gas. The absence of specific physical findings in cases of trapped gas supports this distinction.
Describing Symptoms to a Doctor
When describing your symptoms to a doctor, provide as much detail as possible. Specify the location of the pain (e.g., upper left quadrant, lower right quadrant). Describe the type of pain (e.g., cramping, dull, sharp). Note the duration and frequency of the pain episodes. Include any accompanying symptoms, such as bloating, nausea, or changes in bowel habits.
This detailed information empowers the doctor to make a more accurate assessment.
Key Differences Between IBS Pain and Trapped Gas
| Feature | IBS Pain | Trapped Gas | Diagnostic Considerations |
|---|---|---|---|
| Duration | Can persist for days or weeks | Typically resolves within hours | Length of symptom duration is a significant differentiator. |
| Intensity | Often intense, cramping | Usually milder, intermittent | Pain intensity helps differentiate between the two. |
| Accompanying Symptoms | Bloating, diarrhea, constipation, nausea | Mainly abdominal discomfort | Presence of additional symptoms strongly suggests IBS. |
| Physical Examination | May reveal tenderness or inflammation | Usually shows no specific physical findings | Physical findings, or lack thereof, can support a diagnosis. |
Management Strategies for IBS Pain and Trapped Gas
IBS pain and trapped gas can significantly impact daily life. Fortunately, several effective management strategies can help alleviate symptoms and improve quality of life. These strategies involve lifestyle modifications, dietary adjustments, over-the-counter remedies, and stress management techniques. Understanding the interplay of these factors is key to finding relief.
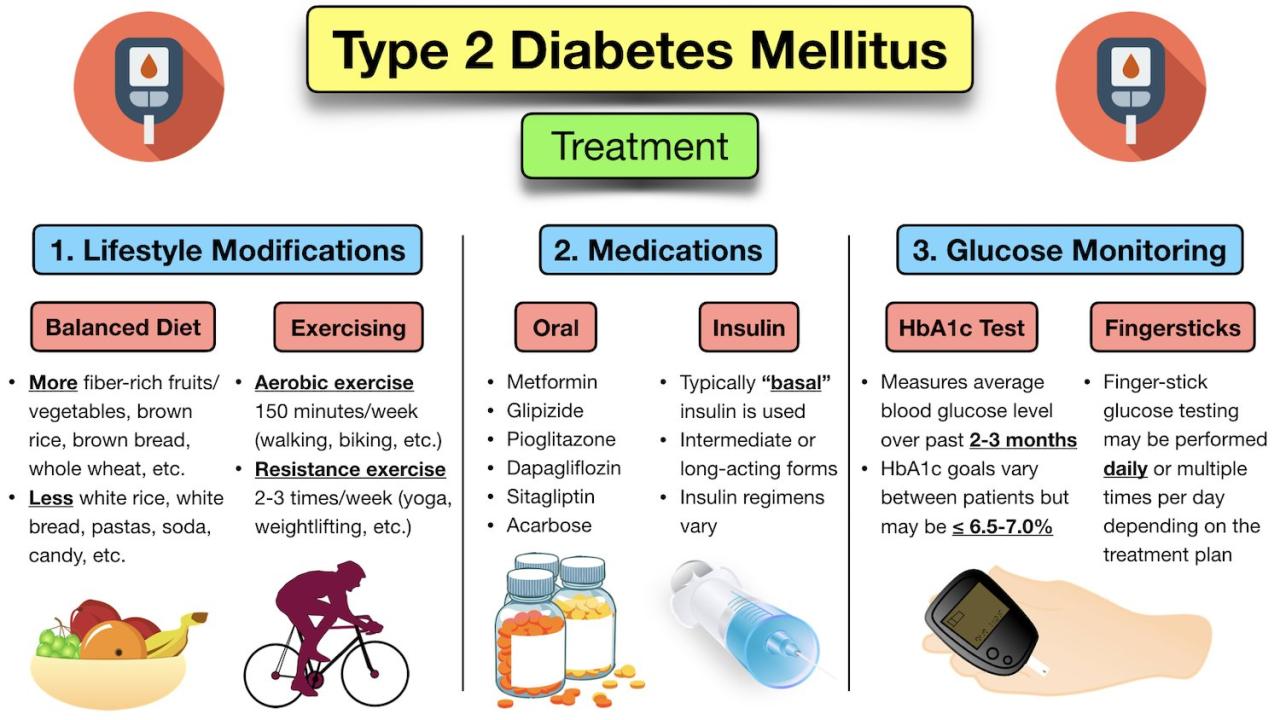
Lifestyle Modifications
Adopting certain lifestyle changes can make a substantial difference in managing IBS symptoms. Regular physical activity, while crucial for overall health, can also contribute to improved digestion. Aim for at least 30 minutes of moderate-intensity exercise most days of the week. Adequate hydration is equally important. Drinking plenty of water helps maintain regularity and can aid in reducing gas buildup.
Getting enough sleep is essential for overall well-being and can positively impact digestion. Maintaining a consistent sleep schedule can contribute to better gut health.
Dietary Recommendations
Dietary modifications play a significant role in managing IBS and trapped gas. Identifying trigger foods is crucial. Common culprits include certain fruits, vegetables, dairy products, and processed foods. Keeping a food diary can help pinpoint specific dietary elements that exacerbate symptoms. Gradually introducing potentially problematic foods, monitoring reactions, and noting symptom patterns can help in creating a personalized dietary plan.
Ugh, those pesky IBS pains or trapped gas. It’s frustrating, isn’t it? Sometimes, it feels like the root cause is hidden, like a mystery waiting to be solved. Learning about conditions like congenital adrenal hyperplasia might offer a surprising connection to some of those digestive issues. For a deeper dive into congenital adrenal hyperplasia overview, check out this informative article: congenital adrenal hyperplasia overview.
Even if it’s not the answer, understanding more about different potential underlying factors can help us better manage those frustrating IBS symptoms.
Eating smaller, more frequent meals throughout the day can help prevent digestive overload. Chewing food thoroughly can improve digestion and reduce gas production.
Over-the-Counter Medications and Supplements
Several over-the-counter medications and supplements can provide relief from IBS symptoms. Fiber supplements can help regulate bowel movements and reduce bloating. Choose a supplement with a slow-release mechanism to avoid digestive discomfort. Probiotics, which are live microorganisms, can positively influence gut health and potentially alleviate symptoms. Consult with a healthcare professional before incorporating any new supplements.
Over-the-counter pain relievers, like ibuprofen, can be effective in managing pain. However, overuse should be avoided.
Stress Management Techniques
Stress is a significant contributor to IBS symptoms. Stress management techniques are therefore important. Practices like yoga, meditation, deep breathing exercises, and mindfulness can effectively reduce stress levels. Identifying stressors and developing healthy coping mechanisms can lead to improved overall well-being and symptom management. Prioritizing relaxation and stress reduction can significantly impact IBS symptoms.
Sample Daily Diet Plan for Managing IBS and Trapped Gas
| Meal | Food Items | Description | Potential Impact |
|---|---|---|---|
| Breakfast | Oatmeal with berries and a small amount of almond milk | A balanced breakfast that provides fiber and antioxidants. | May promote regularity and reduce bloating. |
| Lunch | Grilled chicken salad with mixed greens, cucumber, and quinoa | A light and easily digestible lunch. | Provides protein and fiber without potential digestive triggers. |
| Dinner | Baked fish with roasted vegetables (broccoli, carrots, and sweet potato) | A lean protein source with healthy vegetables. | A generally well-tolerated meal that provides essential nutrients. |
| Snacks | Plain yogurt with a sprinkle of granola, apple slices with almond butter | Healthy snacks that offer protein, fiber, and healthy fats. | Can help maintain stable blood sugar and prevent digestive upset. |
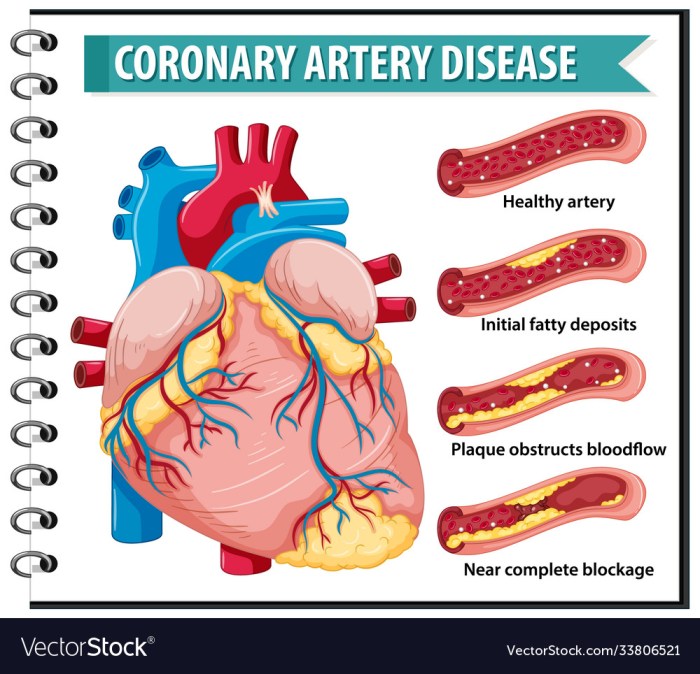
Exploring Underlying Medical Conditions
Understanding IBS pain and trapped gas is crucial, but sometimes, these symptoms can be a sign of something more serious. Underlying medical conditions can mimic the symptoms of irritable bowel syndrome (IBS) and trapped gas, making it challenging to pinpoint the true cause. Accurate diagnosis requires a careful evaluation of symptoms, medical history, and potential contributing factors.While IBS is often a functional disorder, meaning no specific physical abnormality is found, other conditions can manifest with remarkably similar symptoms.
This necessitates a thorough assessment to rule out potential underlying causes and ensure appropriate management. The information below highlights conditions that might present with comparable symptoms, emphasizing the importance of seeking medical attention for persistent or worsening symptoms.
Conditions Mimicking IBS and Trapped Gas Symptoms
Many conditions can mimic the symptoms of IBS and trapped gas. Careful evaluation and diagnostic testing are essential for identifying the underlying cause and ensuring appropriate treatment.
| Condition | Symptoms | Potential Causes | Diagnostic Procedures |
|---|---|---|---|
| Crohn’s Disease | Abdominal pain, cramping, diarrhea, fever, weight loss, fatigue, and sometimes blood in the stool. | Inflammation of the digestive tract, often triggered by immune system response or environmental factors. | Colonoscopy with biopsies, blood tests (CBC, CRP), stool tests (for blood and infection). |
| Ulcerative Colitis | Bloody diarrhea, abdominal pain, fever, weight loss, and fatigue. | Inflammation of the colon and rectum, likely autoimmune-related. | Colonoscopy with biopsies, blood tests (CBC, CRP), stool tests (for blood and infection). |
| Inflammatory Bowel Disease (IBD) | Recurring abdominal pain, diarrhea, weight loss, fever, fatigue, and possible rectal bleeding. | A chronic inflammatory condition of the gastrointestinal tract, including Crohn’s and ulcerative colitis. | Colonoscopy with biopsies, blood tests (CBC, CRP), stool tests, and possibly imaging studies (CT scan). |
| Ovarian Cysts | Abdominal pain, bloating, cramping, and pressure, which can be mistaken for trapped gas. Symptoms often worsen during menstruation. | Fluid-filled sacs that develop on or within the ovaries. | Pelvic exam, transvaginal ultrasound, blood tests (hormone levels), and possibly CT scan or MRI. |
| Appendicitis | Sudden onset of pain, typically localized to the lower right abdomen, nausea, vomiting, and fever. | Inflammation of the appendix, usually caused by obstruction. | Physical examination, blood tests (CBC, CRP), imaging studies (ultrasound, CT scan). |
| Gallstones | Abdominal pain, often in the upper right quadrant, nausea, vomiting, and fever. | Hard deposits that form in the gallbladder. | Physical examination, blood tests (liver function tests), imaging studies (ultrasound, CT scan). |
Importance of Seeking Medical Attention
Persistent or worsening symptoms, particularly those that significantly impact daily life, require immediate medical attention. Delayed diagnosis or treatment of underlying conditions can lead to serious complications. It’s crucial to consult a healthcare professional for a comprehensive evaluation and appropriate management.
Relevant Tests and Investigations
Various tests and investigations can help identify underlying conditions that mimic IBS or trapped gas. These may include blood tests to assess inflammation markers, stool tests to check for infections or blood, imaging studies (such as X-rays, CT scans, or ultrasounds) to visualize the digestive tract, and endoscopic procedures (such as colonoscopies or endoscopies) to examine the lining of the digestive organs.
The specific tests will be determined by the healthcare provider based on the individual’s symptoms and medical history.
Self-Care and Coping Mechanisms
Managing IBS pain and trapped gas goes beyond just medication and dietary changes. A crucial component of effective symptom management is self-care and developing coping mechanisms. By actively addressing stress and cultivating healthy habits, individuals can significantly improve their overall well-being and reduce the impact of these conditions on their daily lives.Self-care strategies are not a luxury but a necessity for individuals with IBS.
Taking proactive steps to manage stress, improve relaxation, and foster a supportive environment can empower individuals to better control their symptoms and lead fulfilling lives. These techniques are not intended to replace medical advice or professional treatment but are rather complementary approaches that can significantly enhance symptom management.
Ugh, those pesky IBS pains or trapped gas bubbles can be seriously debilitating. It’s easy to jump to conclusions, especially when discomfort strikes, but sometimes it’s just a tricky digestive issue. It’s important to remember that STDs aren’t always a sign of infidelity, as you can learn more about at this helpful resource. So, next time you’re dealing with digestive distress, try not to let your mind wander down unnecessary paths.
Focus on finding the right relief for your specific symptoms.
Relaxation Techniques
Effective relaxation techniques can significantly reduce the intensity of IBS symptoms. These techniques work by decreasing the body’s physiological stress response, promoting relaxation, and reducing the frequency and severity of pain episodes. Various relaxation techniques can be integrated into daily routines to achieve these goals.Deep breathing exercises, for instance, are a simple and readily accessible way to calm the nervous system.
Incorporating slow, deep breaths can help regulate heart rate and blood pressure, reducing feelings of anxiety and tension that can exacerbate IBS symptoms. Progressive muscle relaxation, a technique involving tensing and releasing different muscle groups, can also be beneficial. This method helps individuals become more aware of physical tension and develop strategies to release it. Meditation, another valuable tool, encourages mindfulness and focus, helping individuals to detach from anxious thoughts and promote a sense of calm.
Stress Reduction Techniques
Chronic stress can exacerbate IBS symptoms. Understanding the link between stress and IBS symptoms is crucial for developing effective coping strategies. Stress reduction techniques are vital tools in managing the condition.Yoga and Tai Chi are examples of practices that combine physical postures, controlled breathing, and mindfulness to reduce stress and promote relaxation. These practices can help improve flexibility, reduce muscle tension, and calm the mind, leading to a reduction in IBS symptoms.
Mindfulness-based stress reduction (MBSR) programs are also beneficial, as they equip individuals with techniques to observe their thoughts and feelings without judgment, which can be helpful in managing stress and anxiety. Consistent practice of these techniques can foster a sense of inner peace, reducing the triggers that can exacerbate IBS symptoms.
Home Management Tips
Creating a supportive home environment can significantly impact IBS management. Following these tips can make a substantial difference in reducing the impact of IBS pain and trapped gas on daily life.
- Establish a regular sleep schedule:
- Maintain a food journal:
- Create a relaxing bedtime routine:
- Engage in regular physical activity:
Adequate sleep is crucial for overall well-being and can directly impact symptom management. A consistent sleep schedule helps regulate the body’s natural rhythms, potentially reducing IBS-related discomfort.
Keeping track of what you eat and how your body responds can help identify potential triggers and dietary patterns that exacerbate symptoms. This awareness can help you make informed choices and tailor your diet to minimize IBS-related discomfort.
A calming bedtime routine, such as taking a warm bath, reading a book, or listening to relaxing music, can help promote better sleep and reduce stress levels, ultimately influencing IBS symptom management.
Regular exercise, even moderate activity, can improve digestion and reduce stress, which can be helpful in managing IBS symptoms. However, it’s important to consult with a doctor before starting any new exercise routine.
The Importance of a Supportive Social Network
A supportive social network is essential for individuals coping with IBS. A strong support system provides emotional comfort, practical assistance, and shared understanding.A strong support network can help individuals feel less isolated and more empowered in managing their condition. Sharing experiences and connecting with others who understand can provide a sense of community and belonging, reducing feelings of stigma and isolation.
This can significantly impact mental well-being and contribute to a more positive outlook on managing IBS. This support can come from family, friends, support groups, or online communities.
Seeking Professional Help
Persistent IBS pain or trapped gas can significantly impact daily life. While self-care strategies are valuable, sometimes professional guidance is necessary to address the underlying causes and develop effective management plans. Seeking help from a healthcare professional is a proactive step toward improving your well-being and finding relief.Understanding the process of seeking professional help empowers you to take control of your health journey and navigate the healthcare system confidently.
A collaborative approach between you and your healthcare provider is crucial for successful management of your symptoms.
Steps to Seeking Professional Help
Seeking professional help is a multi-step process. Start by identifying a healthcare provider who can address your concerns. This could be your general practitioner (GP) or a gastroenterologist, a specialist in digestive health. A thorough evaluation will involve assessing your symptoms, medical history, and lifestyle factors.
- Initial Consultation with Your GP: Your GP can provide an initial evaluation and determine if a referral to a gastroenterologist is necessary. They can also help you understand your symptoms and rule out other potential conditions.
- Referral to a Gastroenterologist (if needed): If your GP suspects IBS or recommends further investigation, they can refer you to a gastroenterologist. This specialist is equipped to handle complex digestive issues and provide specialized care.
- Scheduling Appointments: Contact the chosen healthcare provider’s office to schedule an appointment. Be prepared to provide details about your symptoms, including their duration, frequency, and severity. Prepare questions you want answered.
- Preparing for Consultations: Gather information that may be helpful to your doctor. Keep a detailed symptom diary, noting the times, duration, and intensity of your pain, any triggers, and associated symptoms. Include a list of all medications, supplements, and over-the-counter remedies you’re taking.
- Importance of Detailed Records: A detailed record of your symptoms is essential for accurate diagnosis and treatment planning. This information helps healthcare providers understand the patterns and nuances of your IBS, enabling them to create a personalized management plan.
Questions to Ask Your Doctor
Thorough communication with your doctor is key to effective treatment. Preparing a list of questions will help you get the most out of your consultations. The following table provides examples of questions categorized for clarity:
| Category | Question | Potential Answer | Follow-up |
|---|---|---|---|
| Symptom Details | “Can you explain the difference between IBS pain and trapped gas?” | “IBS pain is often described as cramping, abdominal pain, and changes in bowel habits. Trapped gas is typically associated with bloating and discomfort.” | “How can I differentiate between these symptoms at home?” |
| Diagnostic Tests | “What diagnostic tests might be necessary to confirm IBS?” | “Blood tests, stool tests, and potentially an endoscopy or colonoscopy.” | “What are the risks and benefits of each test?” |
| Treatment Options | “What are the different treatment options for IBS, including dietary modifications?” | “Dietary changes, medication, stress management techniques, and behavioral therapies.” | “Which option would be most suitable for my lifestyle and specific needs?” |
| Lifestyle Modifications | “Are there any lifestyle changes that might help alleviate my symptoms?” | “Stress reduction techniques, regular exercise, and maintaining a consistent sleep schedule.” | “What are some specific recommendations I can implement today?” |
| Medications | “Are there any medications that could help manage my IBS pain?” | “Specific medications for IBS, including antispasmodics, antidepressants, or other treatments.” | “What are the potential side effects of these medications?” |
Conclusive Thoughts
In conclusion, understanding the nuances between IBS pain and trapped gas is crucial for effective self-management. This guide has provided a comprehensive overview, equipping you with the tools to identify potential causes, differentiate symptoms, and implement personalized strategies for relief. Remember, persistent or worsening symptoms always warrant a visit to a healthcare professional. By combining self-care practices with professional guidance, you can take proactive steps toward managing these conditions and improving your overall well-being.