Differential diagnosis confirming your diagnosis is a crucial process in medical decision-making. It involves systematically evaluating various potential causes for a patient’s symptoms, meticulously ruling out possibilities, and ultimately confirming the correct diagnosis. This comprehensive guide delves into the steps involved, from defining the concept to interpreting test results, emphasizing the importance of evidence-based medicine and clear communication throughout the process.
Understanding the various diagnostic tools, including medical history, physical examinations, and investigations, is essential. This process, when meticulously followed, can lead to accurate and timely interventions, improving patient outcomes. We’ll explore common pitfalls, errors to avoid, and showcase real-world case studies to solidify your understanding.
Defining Differential Diagnosis
Differential diagnosis is a crucial step in medical decision-making. It’s the process of systematically considering and evaluating various possible conditions that could explain a patient’s symptoms. By carefully considering a range of potential diagnoses, healthcare professionals can arrive at the most accurate and effective treatment plan. A thorough differential diagnosis process ensures that the right diagnosis is identified and the appropriate treatment is initiated, minimizing the risk of misdiagnosis and ensuring optimal patient outcomes.The process involves a careful evaluation of the patient’s history, physical examination findings, and potentially, diagnostic tests.
This meticulous approach allows healthcare providers to narrow down the possibilities and arrive at a diagnosis. A comprehensive differential diagnosis ensures that no significant condition is overlooked, thus leading to the best possible patient care.
Defining the Process
Differential diagnosis involves systematically considering various possible medical conditions that could explain a patient’s symptoms. It requires a comprehensive understanding of medical knowledge and a meticulous approach to evaluating potential causes. The goal is to narrow down the list of possibilities to a manageable number, ideally identifying the single most likely diagnosis.
Steps in Performing a Differential Diagnosis
The process of differential diagnosis typically follows these steps:
- Gathering Patient Information: This involves obtaining a detailed medical history, including past illnesses, allergies, medications, and family history. A thorough review of systems is essential, including any recent changes in lifestyle, exposure to potential pathogens, or any recent traumas.
- Physical Examination: A complete physical examination is crucial for evaluating the patient’s current physical condition. This includes vital signs, observation of any abnormalities, and assessment of various body systems.
- Review of Diagnostic Tests: This step involves reviewing any existing test results, such as blood work, imaging studies, or other lab findings. These results can offer clues to help narrow down the possibilities.
- Formulating a List of Potential Diagnoses: Based on the information gathered, a list of potential diagnoses is compiled. This list should include conditions that are plausible given the patient’s symptoms and medical history. The list should not be limited to the most obvious diagnoses; all possible diagnoses must be considered.
- Systematically Eliminating Possibilities: This crucial step involves evaluating each diagnosis on the list against the collected data. Conditions that are inconsistent with the patient’s presentation are eliminated. This process often involves comparing the patient’s symptoms with the expected symptoms associated with each potential diagnosis.
- Reaching a Conclusion: After thoroughly evaluating and eliminating possibilities, the most likely diagnosis is identified. This diagnosis is supported by the collected data and should align with the patient’s symptoms and medical history.
Importance of Considering Multiple Potential Diagnoses
Considering multiple potential diagnoses is essential to avoid missing a serious or life-threatening condition. A single-minded approach might lead to overlooking a diagnosis that is less obvious but potentially more severe. Focusing on a narrow range of possibilities might result in missed opportunities for early intervention and appropriate treatment.
Figuring out what’s wrong often involves a differential diagnosis, confirming your suspicions. It’s a crucial process in medical practice, like meticulously examining different possibilities before settling on the correct one. Understanding how many calories does walking burn how many calories does walking burn can be part of a broader health assessment, but it’s not a substitute for a proper differential diagnosis, ensuring a conclusive and accurate medical picture.
Ultimately, a thorough differential diagnosis is key to getting the right treatment and a solid recovery plan.
Rationale for Systematic Elimination
Systematic elimination of potential diagnoses is crucial for ensuring accuracy and avoiding misdiagnosis. By systematically comparing each diagnosis with the collected data, healthcare professionals can objectively assess the likelihood of each condition. This approach minimizes the risk of overlooking a serious condition or misinterpreting symptoms.
Flowchart of Differential Diagnosis
| Step | Action |
|---|---|
| 1 | Gather patient information (history, symptoms) |
| 2 | Perform physical examination |
| 3 | Review diagnostic tests (labs, imaging) |
| 4 | Formulate a list of potential diagnoses |
| 5 | Evaluate each diagnosis against collected data |
| 6 | Eliminate inconsistent diagnoses |
| 7 | Identify the most likely diagnosis |
Confirming a Diagnosis
Pinpointing the precise cause of a patient’s symptoms is a crucial step in providing effective treatment. A confirmed diagnosis allows healthcare professionals to tailor therapies to the specific condition, leading to better patient outcomes. This process often involves a combination of methods, from meticulous physical examinations to advanced laboratory tests and imaging techniques.Confirming a suspected diagnosis goes beyond simply identifying symptoms.
It necessitates a careful evaluation of the gathered information, considering the patient’s medical history, physical presentation, and results from various diagnostic tools. This comprehensive approach minimizes the risk of misdiagnosis and ensures that the chosen treatment plan addresses the root cause of the problem.
Methods of Diagnostic Confirmation
The process of confirming a suspected diagnosis frequently involves a multi-faceted approach. This strategy allows for a more complete picture of the patient’s condition, increasing the accuracy of the diagnosis. Multiple methods, each with its own strengths and limitations, are employed.
Imaging Techniques
Imaging techniques play a significant role in visualizing internal structures and identifying potential abnormalities. X-rays, CT scans, MRIs, and ultrasounds are common imaging modalities used to confirm or rule out various conditions. For example, a chest X-ray can reveal pneumonia, while an MRI can identify tumors in the brain.
Laboratory Tests
Laboratory tests provide crucial insights into the patient’s physiological state. Blood tests, urine tests, and other specialized analyses can detect abnormalities in blood counts, hormone levels, or specific markers associated with certain diseases. Elevated levels of certain enzymes, for example, may indicate liver damage.
Physical Examinations
Physical examinations remain a cornerstone of the diagnostic process. A thorough physical exam allows healthcare professionals to assess the patient’s overall health, including vital signs, neurological function, and physical characteristics. Physical examination findings often correlate with suspected diagnoses, providing further evidence for confirmation. For instance, a fever and cough may suggest a respiratory infection.
Comparing Diagnostic Tests
| Test | Description | Reliability | Limitations |
|---|---|---|---|
| X-ray | Uses ionizing radiation to produce images of internal structures. | High for detecting bone fractures and some lung conditions. | Limited in soft tissue visualization. |
| CT Scan | Combines X-ray images from multiple angles to create cross-sectional views. | High for visualizing internal organs and detecting tumors. | Higher radiation exposure than X-rays. |
| MRI | Uses magnetic fields and radio waves to create detailed images of soft tissues. | Excellent for visualizing soft tissues and identifying subtle abnormalities. | Can be time-consuming and may not be suitable for patients with certain metal implants. |
| Blood Tests | Analyze various components of blood, such as cell counts and chemical levels. | High for detecting infections, inflammatory conditions, and organ dysfunction. | Results may be influenced by factors like recent meals or medications. |
Methods for Differential Diagnosis
Differential diagnosis is a crucial process in medicine, requiring careful consideration of various factors to arrive at the most accurate and appropriate treatment plan. It’s a systematic approach to distinguishing between different possible conditions that could be causing a patient’s symptoms. By meticulously evaluating patient data, clinicians can narrow down the potential causes and focus on the most likely diagnosis.
This process involves a multifaceted investigation that considers the patient’s history, physical examination, and relevant investigations.This systematic approach helps in avoiding misdiagnosis and ensures that the patient receives the most effective and appropriate care. It’s a dynamic process, constantly adapting as new information emerges during the evaluation.
Common Diagnostic Tools
A variety of tools are used to narrow down the possibilities in a differential diagnosis. These tools range from gathering detailed medical history to conducting physical examinations and ordering relevant investigations. Each tool plays a critical role in the overall assessment and contributes to a comprehensive understanding of the patient’s condition.
- Medical History: A detailed medical history is essential for understanding the patient’s past experiences and potential risk factors. This includes information on previous illnesses, surgeries, allergies, medications, and family history of diseases. A comprehensive history helps establish a baseline understanding of the patient’s health status and identifies potential contributing factors to the current condition.
- Physical Examination: A thorough physical examination is crucial for assessing the patient’s current physical status. This involves evaluating vital signs, observing physical characteristics, listening to the heart and lungs, and palpating various body parts to identify any abnormalities or signs of disease. Findings from the physical examination, combined with the medical history, contribute significantly to narrowing the differential diagnosis.
- Investigations: Investigations such as blood tests, imaging studies (X-rays, CT scans, MRIs), and other specialized tests provide objective data that can aid in confirming or ruling out specific diagnoses. The choice of investigations depends on the suspected conditions based on the patient’s history and physical examination.
Role of Symptoms, Signs, and Risk Factors
Symptoms, signs, and risk factors all play a significant role in the differential diagnosis process. Symptoms are subjective experiences reported by the patient, while signs are objective observations made by the clinician during the physical examination. Risk factors are conditions or exposures that increase the likelihood of developing a particular disease. Understanding these factors is critical in identifying potential underlying causes and refining the differential diagnosis.
- Symptoms: Symptoms provide valuable clues about the nature of the condition. For example, persistent cough could indicate various respiratory problems, while sudden onset of severe headache might suggest a neurological issue. Careful analysis of symptom characteristics, such as duration, frequency, and intensity, is essential.
- Signs: Signs are objective manifestations of disease, observable by the clinician. For example, fever, rash, or swelling are signs that may indicate an infection or other underlying condition. These objective findings support or contradict the patient’s reported symptoms.
- Risk Factors: Identifying risk factors, such as smoking history, exposure to certain chemicals, or family history of a particular disease, can significantly narrow the range of possible diagnoses. For example, a patient with a family history of heart disease and high blood pressure is at a higher risk for cardiovascular problems.
Structured Approach to Evaluating Patient Data
A structured approach to evaluating patient data is essential for a thorough differential diagnosis. This includes systematically gathering and analyzing information from various sources, including the patient’s history, physical examination, and investigations. This structured approach helps maintain focus and ensures no relevant piece of information is overlooked.
- Prioritizing Information: Gathering all information about the patient and then prioritizing the relevant pieces of information, such as symptoms, risk factors, and signs. This prioritization helps to focus the diagnostic process.
- Formulating Hypotheses: Formulating possible diagnoses based on the gathered data. This process involves considering potential causes, based on the patient’s symptoms, risk factors, and signs.
- Refining Hypotheses: Refining the list of possible diagnoses by comparing the gathered data to the characteristics of each potential condition. This step involves eliminating diagnoses that are unlikely given the patient’s presentation.
Example Diagnostic Table
The following table provides examples of common symptoms, potential causes, and associated diagnostic tests.
| Symptom | Possible Causes | Diagnostic Tests |
|---|---|---|
| Persistent cough | Bronchitis, pneumonia, asthma, lung cancer | Chest X-ray, sputum analysis, pulmonary function tests |
| Severe headache | Migraine, tension headache, brain tumor, meningitis | Neurological examination, CT scan of the head, blood tests |
| High fever | Viral infection, bacterial infection, autoimmune disease | Blood tests (CBC, cultures), urinalysis, imaging studies |
Evidence-Based Confirmation
Evidence-based medicine (EBM) plays a crucial role in confirming a suspected diagnosis. It bridges the gap between clinical experience and rigorous scientific investigation, ensuring diagnoses are supported by robust data and not just subjective opinions. This approach allows for more accurate and consistent care for patients.The process of confirming a diagnosis using EBM involves carefully considering the available research evidence, including clinical practice guidelines and peer-reviewed studies.
This evidence helps refine diagnostic accuracy and provides a framework for choosing the most appropriate treatment strategies. Importantly, EBM recognizes the uniqueness of each patient, emphasizing that while evidence guides care, individual characteristics must also be considered.
Clinical Practice Guidelines
Clinical practice guidelines offer structured recommendations for diagnosing and managing various medical conditions. These guidelines are developed by expert panels and are informed by systematic reviews of existing research. They provide a standardized approach, enhancing the consistency and quality of care across different healthcare settings. For example, guidelines for diagnosing appendicitis Artikel specific criteria for assessing pain, tenderness, and other symptoms.
These guidelines, when used in conjunction with a thorough patient history and physical examination, help clinicians reach a more accurate diagnosis.
Research Studies
Research studies, particularly randomized controlled trials (RCTs), provide strong evidence for the effectiveness of diagnostic tests and treatments. RCTs involve comparing different diagnostic approaches or treatments, allowing researchers to isolate the effects of specific interventions. For example, a study might compare the accuracy of different imaging modalities in detecting a particular type of tumor. Such research helps determine the most reliable and efficient methods for diagnosis.
Patient-Specific Considerations
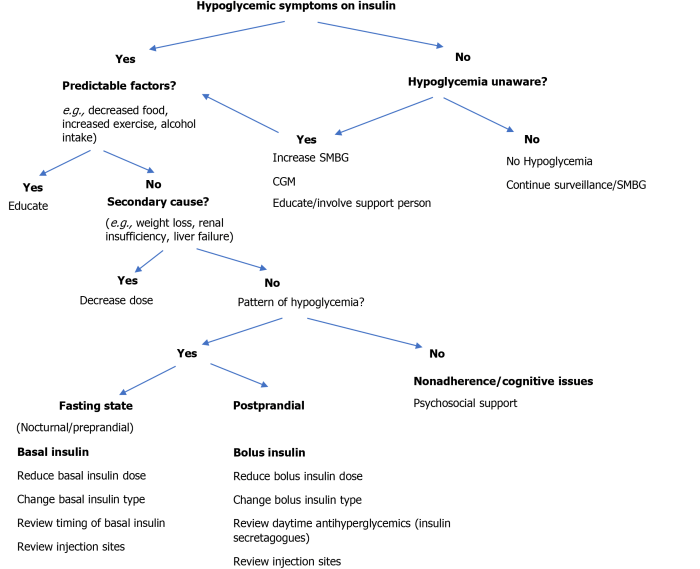
While evidence-based medicine provides a solid foundation, the patient’s unique characteristics must be carefully considered during the confirmation process. Factors such as age, sex, comorbidities, and family history can significantly influence the presentation and severity of a condition. For example, a patient with a history of diabetes might exhibit different symptoms of heart disease compared to a patient without this pre-existing condition.
Thus, a thorough understanding of the patient’s medical history is vital to interpret research findings within the context of their specific situation.
Structured Evidence Organization
A structured approach to organizing evidence is crucial for a comprehensive confirmation process. This approach involves documenting all the supporting and refuting evidence in a clear and organized format. A table can be a useful tool for this purpose.
| Potential Diagnosis | Supporting Evidence | Refuting Evidence | Patient-Specific Considerations |
|---|---|---|---|
| Appendicitis | Right lower quadrant pain, tenderness, elevated white blood cell count | Absence of fever, normal bowel sounds | Age: 20-year-old female; history of irritable bowel syndrome |
| Ovarian Cyst | Pelvic pain, irregular menstrual cycle | Normal bowel sounds, absence of fever | Age: 25-year-old female; history of prior ovarian cysts |
This table demonstrates a structured approach to documenting supporting and refuting evidence for different potential diagnoses. The inclusion of patient-specific factors highlights the importance of individualized consideration in the confirmation process.
Case Studies and Examples
Diving deeper into the practical application of differential diagnosis, case studies offer a real-world window into the process. They illuminate how clinicians systematically evaluate a patient’s symptoms, consider various possibilities, and ultimately arrive at a definitive diagnosis. This section will showcase a detailed case study, demonstrating the entire process from symptom presentation to confirmation.
Patient Presentation
A 35-year-old female presented to the clinic complaining of persistent headaches, nausea, and sensitivity to light. She reported a recent history of fever and fatigue. Physical examination revealed mild neck stiffness and a slight elevation in temperature. No other significant findings were noted.
Considering Possible Diagnoses
The presenting symptoms suggested a range of potential diagnoses, including meningitis, migraine, or even a viral infection. Each possibility demanded further investigation to differentiate it from the others. The differential diagnosis list included:
- Meningitis: Characterized by inflammation of the meninges, often associated with fever, headache, and neck stiffness. The patient’s symptoms aligned somewhat with this diagnosis.
- Migraine: A common neurological disorder frequently presenting with severe headaches, nausea, and photophobia. The recent history of fever and fatigue suggested against this diagnosis.
- Viral Infection: Viral infections can cause a variety of symptoms, including fever, headache, and fatigue. The combination of symptoms pointed towards this as a possible diagnosis.
Diagnostic Procedures
To confirm or rule out each possibility in the differential diagnosis, several diagnostic procedures were implemented. These included:
- Complete Blood Count (CBC): To assess for infection and rule out other blood-related issues.
- Lumbar Puncture (LP): To analyze cerebrospinal fluid (CSF) for evidence of infection. A critical step in distinguishing meningitis from other conditions.
- Neurological Examination: To further evaluate neurological function and rule out any other neurological abnormalities.
Confirmation of Diagnosis
The results of the diagnostic procedures were crucial in confirming the diagnosis. The CBC revealed a mild elevation in white blood cells, suggesting an inflammatory process. The lumbar puncture showed elevated protein levels and increased white blood cell counts in the CSF, strongly indicative of meningitis. The neurological examination was unremarkable beyond the neck stiffness. No other abnormalities were detected.
Table: Differential Diagnosis and Confirmation
| Possible Diagnosis | Supporting Symptoms | Confirmatory Tests | Results | Diagnosis Status |
|---|---|---|---|---|
| Meningitis | Headache, nausea, photophobia, fever, neck stiffness | CBC, LP, Neurological exam | Elevated WBCs, elevated protein & WBCs in CSF, normal neurological exam except neck stiffness | Confirmed |
| Migraine | Headache, nausea, photophobia | CBC, neurological exam | Normal CBC, normal neurological exam, absence of fever | Excluded |
| Viral Infection | Headache, fatigue, fever | CBC | Mildly elevated WBCs | Possible, but further tests ruled out other possibilities |
Interpreting Test Results: Differential Diagnosis Confirming Your Diagnosis
Deciphering the meaning behind diagnostic test results is crucial for accurate diagnoses. A single test result, in isolation, can be misleading. Understanding the limitations of the test, the potential for errors, and the interplay of multiple factors is essential to avoid misinterpretations and ensure appropriate patient care. This section delves into the nuances of interpreting test results, highlighting the importance of context and the need for a holistic approach.
Limitations of Diagnostic Tests
Diagnostic tests, while valuable tools, are not infallible. Each test possesses inherent limitations, including the possibility of false positives or false negatives. Factors such as the test’s sensitivity and specificity, the patient’s individual characteristics, and the testing environment can all influence the accuracy of the results. Recognizing these limitations is critical to avoiding misdiagnosis and ensuring appropriate treatment plans.
Multiple Tests for Support
A single diagnostic test rarely provides sufficient evidence for a definitive diagnosis. The use of multiple, complementary tests is often necessary to build a comprehensive picture of the patient’s condition. These tests should target different aspects of the suspected pathology, corroborating findings and reducing the likelihood of misinterpretation. For example, a combination of blood tests, imaging studies, and physical examinations can provide a more complete understanding of a patient’s condition compared to relying on any one method alone.
Factors in Interpreting Results
Several factors contribute to the interpretation of test results. These factors include the patient’s medical history, symptoms, physical examination findings, and other laboratory data. The context surrounding the test is crucial. For instance, a high blood pressure reading in a patient with a known history of hypertension might be interpreted differently than in a patient without such a history.
Consideration of these factors is vital for accurate interpretation.
Examples of Misinterpretation
Misinterpretations of test results can lead to significant errors in diagnosis and treatment. For example, a slightly elevated liver enzyme level in a patient taking certain medications might be incorrectly attributed to liver disease. Furthermore, a negative result on a specific test does not always rule out a condition, as there may be other factors influencing the test outcome.
The presence of confounding variables, such as medication use, dietary factors, or recent infections, can impact test results and must be carefully considered. Understanding the potential for these errors is paramount.
Test Results and Clinical Significance
| Test Result | Clinical Significance |
|---|---|
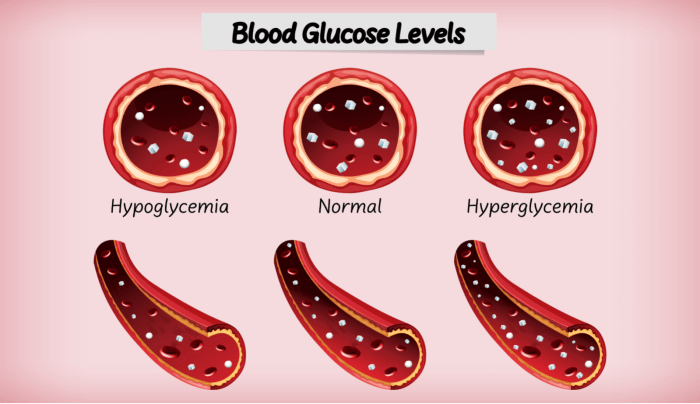
| Elevated blood glucose level (fasting) | Suggests diabetes or pre-diabetes. Further investigation with oral glucose tolerance test (OGTT) is required for confirmation. |
| Elevated white blood cell count | Suggests infection or inflammation. Additional tests to identify the source of infection may be necessary. |
| Abnormal chest X-ray | Suggests potential lung disease or other thoracic abnormalities. Further imaging studies (CT scan) may be required. |
| Negative HIV antibody test | Does not rule out HIV infection. Further testing (e.g., Western blot) is needed for confirmation, particularly in cases with high clinical suspicion. |
| Low hemoglobin | Suggests anemia. Further tests (e.g., iron studies) are necessary to determine the underlying cause. |
Understanding the limitations of diagnostic tests and the potential for misinterpretation is vital in patient care. The careful consideration of multiple tests and the context of the patient’s overall clinical picture are crucial for accurate diagnoses.
Communication and Documentation
Effective communication and meticulous documentation are cornerstones of accurate differential diagnosis. These processes ensure a cohesive and comprehensive approach to patient care, enabling informed decision-making and improved patient outcomes. Clear communication bridges gaps between healthcare professionals, allowing for a shared understanding of the patient’s condition and facilitating a unified approach to diagnosis and treatment. Thorough documentation, in turn, provides a detailed record of the diagnostic journey, serving as a valuable resource for future reference, quality improvement, and legal protection.Effective communication is essential for a smooth and collaborative diagnostic process.
This process involves active listening, clear articulation of observations, and respectful exchange of information. When healthcare professionals communicate effectively, they can efficiently share information, discuss potential diagnoses, and coordinate care, thereby maximizing the chance of a timely and accurate diagnosis.
Importance of Clear Communication Between Healthcare Professionals
Clear communication fosters collaboration and avoids misinterpretations. When information is shared effectively, different specialists can contribute their expertise and perspectives to build a complete picture of the patient’s condition. This collaborative approach leads to a more comprehensive and nuanced understanding of the case, enhancing the likelihood of arriving at the correct diagnosis. This is especially crucial in complex cases involving multiple specialists, such as cardiology, neurology, and pulmonology.
Importance of Detailed Documentation of the Diagnostic Process
Detailed documentation is crucial for tracking the diagnostic process. It provides a chronological record of all assessments, investigations, and findings. This meticulous documentation serves as a valuable reference point for future consultations, allowing healthcare professionals to quickly access and review relevant information, ensuring continuity of care and reducing potential errors. Moreover, it is essential for legal purposes, as it can act as evidence in cases of disputes or litigation.
Use of Medical Terminology in Documentation
Consistent use of precise medical terminology is essential in documentation. This ensures that the information is unambiguous and easily understood by other healthcare professionals. Using standardized medical terminology minimizes ambiguity and facilitates accurate interpretation of the documented findings. This promotes interprofessional communication, ensuring everyone is on the same page, which is paramount in complex cases.
Importance of Sharing Diagnostic Reasoning with the Patient
Transparency in the diagnostic process builds trust and empowers patients. Explaining the diagnostic reasoning, including the differential diagnoses considered, provides patients with a clear understanding of their condition and the rationale behind the chosen course of action. This shared understanding fosters collaboration and allows patients to actively participate in their care, improving treatment adherence and satisfaction.
Figuring out what’s wrong, especially with a complex condition like type 2 diabetes, often involves a differential diagnosis. This process helps confirm your diagnosis, and access to the right care is crucial. For instance, ensuring you have the right support for managing type 2 diabetes, including access to access to type 2 diabetes care , is vital.
Ultimately, a thorough differential diagnosis helps solidify the right treatment plan.
Sample Documentation Format for the Differential Diagnosis Process
| Date | Time | Healthcare Professional | Observations | Differential Diagnoses | Investigations | Results | Reasoning | Diagnosis |
|---|---|---|---|---|---|---|---|---|
| 2024-10-27 | 10:00 AM | Dr. Smith | Patient presented with fever, cough, and shortness of breath. | Pneumonia, Bronchitis, Influenza | Chest X-ray, Blood tests | Chest X-ray: Bilateral infiltrates; Blood tests: Elevated WBC count | The presence of bilateral infiltrates on the chest X-ray, coupled with elevated white blood cell count, suggests pneumonia as the most likely diagnosis. | Pneumonia |
Potential Pitfalls and Errors
Navigating the complexities of differential diagnosis is a delicate dance, requiring meticulous attention to detail and a critical eye. While the process aims for precision, pitfalls and errors can occur, leading to misdiagnosis and potentially serious consequences. Understanding these common errors and the factors that contribute to them is crucial for improving diagnostic accuracy and patient care.
Common Errors in Differential Diagnosis
Errors in differential diagnosis often stem from a combination of factors, including inadequate patient history, limited physical examination, insufficient diagnostic testing, and cognitive biases. A thorough and systematic approach to diagnosis is essential to mitigate these risks.
Factors Leading to Misdiagnosis
Several factors can contribute to misdiagnosis, ranging from systemic issues within healthcare systems to individual cognitive biases. Insufficient resources, time constraints, and communication breakdowns can hinder the diagnostic process. Also, diagnostic fatigue, a phenomenon where clinicians become less attentive due to a high volume of cases, can lead to overlooking subtle clues.
Figuring out what’s causing your tummy troubles often involves a differential diagnosis, confirming your initial suspicions. While this process is important, sometimes simple lifestyle changes can be just as effective. For example, incorporating certain foods into your diet can really help soothe Irritable Bowel Syndrome (IBS) symptoms. Check out these 6 foods to help soothe IBS symptoms naturally here.
Ultimately, a proper differential diagnosis is crucial for pinpointing the root cause of your discomfort.
Role of Biases in Diagnostic Reasoning
Cognitive biases can significantly influence the diagnostic process. Confirmation bias, for example, involves favoring information that confirms pre-existing hypotheses while disregarding contradictory evidence. Anchoring bias, where clinicians rely too heavily on initial impressions, can also lead to misdiagnosis. Availability heuristic, where clinicians rely on readily available information, can lead to inaccurate assessments. These biases highlight the importance of a systematic approach to diagnosis, emphasizing the need for critical evaluation of all available data.
Importance of Critical Thinking
Critical thinking plays a vital role in avoiding errors in differential diagnosis. It involves evaluating information objectively, questioning assumptions, and considering alternative explanations. Critical thinkers are less susceptible to cognitive biases and more adept at recognizing patterns and inconsistencies in data. Developing strong critical thinking skills is essential for accurate and effective diagnostic reasoning.
Potential Pitfalls and Strategies for Avoiding Them
| Potential Pitfalls | Strategies for Avoiding Them |
|---|---|
| Insufficient Patient History | Employ structured questionnaires, actively seeking details about symptoms, medical history, and social context. |
| Limited Physical Examination | Conduct a comprehensive physical examination, paying close attention to all pertinent systems. Utilize specialized examination techniques as needed. |
| Inadequate Diagnostic Testing | Select appropriate diagnostic tests based on the differential diagnosis, considering their sensitivity, specificity, and cost-effectiveness. |
| Confirmation Bias | Actively seek out contradictory evidence, consider alternative hypotheses, and document all findings meticulously. |
| Anchoring Bias | Encourage the consideration of alternative hypotheses early in the diagnostic process. Re-evaluate initial impressions in light of new information. |
| Diagnostic Fatigue | Implement strategies to maintain focus and alertness during high-volume periods. Ensure adequate breaks and time for reflection. |
| Overreliance on Expert Opinion | While expert opinion is valuable, it should not substitute independent critical analysis. Encourage questioning and challenge of assumptions. |
| Ignoring Subjective Data | Acknowledge and carefully consider subjective data (patient’s perception of symptoms). This may be particularly important in conditions where objective signs are absent or unreliable. |
Illustrative Examples
Differential diagnosis is a cornerstone of effective medical practice. It’s the process of systematically considering various possible conditions that could explain a patient’s symptoms, ultimately leading to an accurate diagnosis. A crucial step in patient care, differential diagnosis ensures appropriate treatment and prevents misdiagnosis, which can have significant implications for patient outcomes.
Common Conditions Requiring Differential Diagnosis
Differential diagnosis is particularly vital in conditions where symptoms overlap considerably. Consider cases of abdominal pain, headaches, or skin rashes. These symptoms can stem from a multitude of causes, ranging from benign conditions to serious illnesses. Properly identifying the underlying cause requires a thorough understanding of each potential condition and its associated symptoms.
Importance of Differential Diagnosis in Specific Conditions
In diagnosing conditions like appendicitis, a careful differential diagnosis is essential to distinguish it from other causes of abdominal pain, such as gastroenteritis or ovarian cysts. Failure to consider these alternatives could lead to delayed or inappropriate treatment, potentially impacting the patient’s health. Similarly, in cases of suspected stroke, differentiating it from transient ischemic attacks (TIAs) is crucial for effective management and preventing potentially devastating consequences.
Overlapping Symptoms and Methods for Distinction
Many medical conditions share similar symptoms. For instance, both influenza and pneumonia can present with fever, cough, and body aches. Distinguishing between these conditions requires careful consideration of additional factors such as the duration of symptoms, presence of chest pain, and results from diagnostic tests like chest X-rays and blood tests. The presence of specific symptoms, the pattern of symptom development, and the results of physical examinations and investigations are key factors.
Case Studies: Comparing and Contrasting Conditions, Differential diagnosis confirming your diagnosis
| Condition 1: Influenza | Condition 2: Pneumonia |
|---|---|
| Symptoms: Fever, cough, body aches, fatigue, sore throat, runny nose. | Symptoms: Fever, cough, body aches, fatigue, shortness of breath, chest pain, productive cough (with phlegm). |
| Duration: Typically 5-7 days. | Duration: Can range from several days to weeks, potentially longer with complications. |
| Diagnostic Tests: Often, no specific tests are needed, but a rapid influenza test may be considered. | Diagnostic Tests: Chest X-ray, blood tests (looking for inflammatory markers), sputum analysis. |
| Treatment: Primarily supportive care, such as rest, fluids, and over-the-counter medications for symptom relief. | Treatment: Often requires antibiotics, and possibly antiviral medications, depending on the causative organism. |
The table above highlights the key differences between influenza and pneumonia. While both can present with similar symptoms, the duration, diagnostic tests, and treatment strategies differ significantly. A careful evaluation of these aspects helps in establishing the accurate diagnosis and guiding the appropriate management strategy. This process is vital for ensuring the best possible patient outcome.
Closing Notes
In conclusion, differential diagnosis confirming your diagnosis is a multifaceted process requiring a systematic approach, critical thinking, and a deep understanding of medical principles. By carefully considering potential diagnoses, utilizing various diagnostic tools, and interpreting results with precision, healthcare professionals can arrive at accurate diagnoses and ensure optimal patient care. Remember, meticulous documentation and clear communication are crucial components of this vital process.