Chlorella superfood omega 3 presents a fascinating opportunity to explore a potential powerhouse of nutrition. This algae, packed with vitamins and minerals, might also offer a unique approach to obtaining omega-3 fatty acids, crucial for overall health. We’ll delve into the science behind chlorella, comparing its omega-3 content to more traditional sources, and examine the potential benefits and drawbacks.
This comprehensive guide will explore the potential of chlorella as an omega-3 source, examining its nutritional profile, potential interactions, and the scientific research surrounding it. We’ll also look at different supplement forms, dosages, and practical ways to incorporate chlorella into a healthy lifestyle.
Introduction to Chlorella and Omega-3s

Chlorella, a single-celled freshwater algae, boasts an impressive nutritional profile, packing a powerful punch of nutrients. This tiny organism is a remarkable source of protein, vitamins, minerals, and antioxidants. It’s often touted as a superfood due to its potential health benefits. Meanwhile, omega-3 fatty acids are essential polyunsaturated fats crucial for various bodily functions, including brain health, heart health, and inflammation regulation.
Understanding the potential interactions between these two powerful nutrients can be beneficial for those seeking holistic wellness.Omega-3 fatty acids come in different forms, each with specific roles in the body. Alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA) are the key players. ALA is an essential fatty acid that the body can convert to EPA and DHA, though this conversion is often inefficient.
EPA and DHA are typically obtained through dietary sources like fatty fish, and are directly beneficial for cardiovascular health, cognitive function, and reducing inflammation. The different forms of omega-3s play unique roles, highlighting the importance of a balanced diet.
Nutritional Profile of Chlorella
Chlorella is a rich source of protein, containing all nine essential amino acids. It also provides a variety of vitamins, including B vitamins, vitamin K, and vitamin C. Furthermore, it’s a good source of minerals such as iron, magnesium, and zinc. This comprehensive nutrient profile contributes to its potential role as a supportive component of a healthy diet.
Chlorella, a superfood packed with omega-3s, is often touted for its potential health benefits. It’s a fascinating ingredient, but when dealing with thyroid issues, like dry mouth symptoms associated with thyroid disease dry mouth , it’s crucial to understand the interplay between these factors. Ultimately, incorporating chlorella into a balanced diet might offer support for overall well-being, but always consult a healthcare professional for personalized advice.
The high chlorophyll content contributes to its distinctive green color and may also play a role in detoxification processes.
Omega-3 Fatty Acid Types and Importance
Omega-3 fatty acids are essential polyunsaturated fats that the body cannot produce on its own. They are crucial for various bodily functions. ALA, EPA, and DHA are the three primary types. ALA is found in plant-based foods, while EPA and DHA are primarily found in fatty fish. The human body can convert ALA to EPA and DHA, but the conversion rate is often low.
Consuming EPA and DHA directly through fish oil supplements or fatty fish can be beneficial.
Potential Link Between Chlorella and Omega-3s
While there isn’t a direct, well-documented interaction between chlorella and omega-3s where chlorella directly produces omega-3 fatty acids, the potential synergistic benefits are intriguing. Chlorella, rich in vitamins and minerals, may support optimal metabolic function, potentially influencing the body’s utilization of omega-3s. Additionally, chlorella is a source of antioxidants, which can help protect omega-3s from oxidation, thus enhancing their bioavailability and efficacy.
Further research is needed to fully understand the extent of this potential synergy.
Benefits Comparison, Chlorella superfood omega 3
| Chlorella Benefits | Omega-3 Benefits | Potential Synergies |
|---|---|---|
| High protein content, all essential amino acids. Excellent source of vitamins and minerals. | Essential for brain health, heart health, and reducing inflammation. Crucial for cell growth and function. | Chlorella’s nutrients may support optimal metabolism, enhancing the body’s ability to utilize omega-3s. Antioxidants in chlorella may protect omega-3s from oxidation. |
| Potential for supporting detoxification processes due to chlorophyll content. | EPA and DHA can support cardiovascular health and reduce triglycerides. | Combined intake might lead to a more comprehensive approach to health support, potentially reducing inflammation and oxidative stress. |
| Rich in antioxidants, which can help protect cells from damage. | Crucial for cognitive function and development, especially in infants and children. | The combination may enhance overall health and well-being by supporting a range of bodily functions. |
Chlorella as a Potential Omega-3 Source
Chlorella, a single-celled green algae, has garnered attention for its potential as a source of various nutrients, including omega-3 fatty acids. While not a primary source in the same way as fish oil, chlorella can contribute to an individual’s omega-3 intake. This section delves into chlorella’s omega-3 content, comparing it to fish oil, and exploring potential mechanisms for its contribution to omega-3 intake.Chlorella, despite its potential, isn’t a significant omega-3 source compared to fatty fish.
Its omega-3 content is relatively low, but it’s important to consider that dietary diversity is crucial for overall health, and chlorella can be part of a balanced nutritional strategy.
Comparison of Chlorella and Fish Oil Omega-3 Content
The omega-3 fatty acids found in chlorella primarily include ALA (alpha-linolenic acid), a precursor to EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid). However, the conversion of ALA to EPA and DHA in the human body is often inefficient. This contrasts significantly with fish oil, which contains EPA and DHA directly, making it a more potent source of these beneficial fatty acids.
Types of Omega-3s in Chlorella
Chlorella primarily contains ALA, a type of omega-3 fatty acid. While ALA is important, it’s not as readily utilized by the body as EPA and DHA, the more potent forms found in fish oil. This difference in bioavailability needs to be considered when assessing the contribution of chlorella to overall omega-3 intake.
Potential Mechanisms for Chlorella’s Omega-3 Contribution
The exact mechanisms through which chlorella contributes to omega-3 intake are still under investigation. However, several factors are considered: chlorella’s unique nutrient profile, including other beneficial compounds, could potentially support the body’s conversion of ALA to EPA and DHA, although the efficiency remains a topic of research. Moreover, the presence of other nutrients in chlorella might indirectly support omega-3 utilization, and further studies are needed to fully understand the intricate interactions.
Comparison Table: Chlorella vs. Fish Oil as Omega-3 Sources
| Feature | Chlorella | Fish Oil |
|---|---|---|
| Primary Omega-3s | ALA | EPA and DHA |
| Bioavailability | Lower; conversion to EPA/DHA is less efficient | High; readily available EPA and DHA |
| Omega-3 Content | Relatively low | High |
| Pros | Potential for additional nutrients, part of a balanced diet | Direct source of EPA and DHA, proven health benefits |
| Cons | Limited contribution to EPA/DHA, conversion efficiency may vary | Potential for high mercury content in some types, cost can vary |
Nutritional Benefits and Potential Drawbacks
Chlorella, a single-celled freshwater algae, boasts a remarkable nutritional profile, often touted for its potential health benefits. Beyond its possible omega-3 content, it offers a wide array of nutrients that contribute to overall well-being. However, like any supplement, chlorella consumption is not without potential drawbacks and interactions. This section explores the multifaceted nature of chlorella, examining both its advantages and potential disadvantages.
Nutritional Profile Beyond Omega-3s
Chlorella is rich in various essential nutrients. It’s a good source of protein, containing all nine essential amino acids. Its high chlorophyll content contributes to its vibrant green color and potentially aids in detoxification processes. Furthermore, chlorella is a substantial source of vitamins and minerals, including vitamins B, C, and K, as well as iron, calcium, and magnesium.
These nutrients play critical roles in various bodily functions, supporting energy production, immune response, and bone health.
Potential Drawbacks and Side Effects
While chlorella is generally considered safe for consumption, some individuals may experience side effects. These can range from mild gastrointestinal issues like bloating, gas, and diarrhea to more severe reactions. Sensitivity to chlorella can vary significantly among individuals, making it crucial to listen to your body and monitor any unusual symptoms.
Potential Interactions with Medications and Supplements
Chlorella can interact with certain medications and supplements. For example, it may interfere with the absorption of certain medications, such as thyroid medications or blood thinners. It’s crucial to consult with a healthcare professional before introducing chlorella into your regimen, especially if you are taking any prescribed medications or supplements. This precaution is essential to avoid potential complications.
A healthcare professional can assess potential interactions and adjust your treatment plan if necessary.
Potential Benefits and Drawbacks for Specific Health Conditions
The following table provides a general overview of the potential benefits and drawbacks of chlorella for different health conditions. It’s essential to understand that this is not exhaustive and individual responses can vary. Consult with a healthcare professional before using chlorella for any specific health condition.
| Health Condition | Potential Benefits | Potential Drawbacks |
|---|---|---|
| Digestive Health | May improve digestive function, reduce bloating and gas in some individuals. | May cause digestive discomfort in others, including diarrhea, gas, or bloating. |
| Iron Deficiency | High in iron, which may help in increasing iron levels, though more research is needed. | May interact with iron supplements or medications. Consult a healthcare professional. |
| Blood Sugar Management | May help in regulating blood sugar levels in some individuals, but further research is necessary. | May interact with blood sugar-lowering medications. Consult a healthcare professional. |
| Weight Management | May aid in weight management due to its high fiber content and potential to increase satiety. | Limited evidence to support this, and may cause digestive issues in some. |
Scientific Research and Studies
While the potential of chlorella as a source of omega-3s is intriguing, the scientific evidence supporting this claim is still relatively limited. Numerous studies investigate the nutritional content of chlorella, but direct exploration of its impact on omega-3 levels in humans or animals remains relatively scarce. This makes it crucial to critically evaluate existing research and understand the methodologies employed to assess the potential benefits accurately.
Review of Existing Studies
The limited research on chlorella’s role in omega-3 production necessitates a careful examination of existing studies. It’s important to recognize that not all studies are created equal, and the methodologies used can significantly impact the interpretation of results. Factors such as the specific chlorella strain used, the duration of the study, the subject population, and the measurement methods all contribute to the validity of findings.
Methodologies Employed in Studies
A variety of methodologies are employed in studies investigating the nutritional composition of chlorella, and these methodologies vary considerably. The most common methods involve analyzing chlorella samples to determine the presence and quantity of different fatty acids, including omega-3s. These analyses typically utilize chromatographic techniques, such as gas chromatography (GC) or high-performance liquid chromatography (HPLC), to separate and identify different fatty acids.
Specific Research Study Example: Impact of Chlorella on Omega-3 Levels
A specific study examining the impact of chlorella on omega-3 levels might involve a controlled feeding trial with laboratory animals (e.g., rats or mice). Researchers would divide the animals into groups, with one group receiving a diet supplemented with chlorella and another group serving as a control. The control group would receive a standard diet without chlorella. The study would last for a defined period, and researchers would regularly analyze the animals’ blood or tissue samples to measure omega-3 fatty acid levels.
Summary of Key Findings
| Study | Chlorella Strain | Duration (weeks/months) | Key Findings | Methodology |
|---|---|---|---|---|
| Example Study 1 | Chlorella vulgaris | 8 weeks | No significant increase in omega-3 levels observed in the chlorella-fed group compared to the control group. | Controlled feeding trial with rats; GC analysis of fatty acid profiles in blood serum. |
| Example Study 2 | Chlorella pyrenoidosa | 12 weeks | Trace amounts of omega-3 fatty acids (e.g., EPA, DHA) detected in chlorella samples but no significant impact on the omega-3 levels in the blood of participants. | Human intervention study; HPLC analysis of blood plasma fatty acids. |
Note: The table above is a hypothetical representation. Actual studies may have different results and methodologies.
Chlorella and Omega-3 Supplements
Chlorella, often touted as a superfood, is increasingly being combined with omega-3 fatty acids in supplement form. This combination aims to leverage the potential health benefits of both ingredients. However, the effectiveness and optimal usage of these combined supplements need careful consideration.The market offers a variety of chlorella omega-3 supplement formulations. Understanding these formulations, their potential benefits, and potential drawbacks is key to making informed choices.
I’ve been exploring chlorella superfood omega 3 lately, and it’s been fascinating to see how it can potentially impact overall health. One thing I’ve noticed is how important it is to maintain good oral health, and sometimes, bumps on the back of your tongue can be a sign of something needing attention. For more information on potential causes of bumps on the back of your tongue, check out this helpful resource: bumps on back of tongue.
Ultimately, incorporating chlorella into a balanced diet might contribute to a healthier mouth and body.
This section delves into the specifics of these products, their effectiveness, and proper usage.
Different Formulations of Chlorella Omega-3 Supplements
Chlorella omega-3 supplements come in various forms, often blending chlorella powder with other ingredients containing omega-3s. Common forms include capsules containing both chlorella and fish oil or algal oil, or tablets combining chlorella with concentrated omega-3 extracts. The different formulations influence the overall product composition and impact on absorption.
Comparison of Effectiveness and Absorption Rates
Comparing the effectiveness and absorption rates of different chlorella omega-3 supplement forms is challenging due to limited, high-quality, controlled studies. While some studies suggest chlorella may enhance the absorption of omega-3 fatty acids, the degree of this enhancement varies based on the specific formulation and individual factors. The presence of other nutrients in the supplement and the overall digestive process influence the body’s ability to utilize the combined ingredients.
Recommended Dosage and Usage Guidelines
Dosage recommendations for chlorella omega-3 supplements vary significantly depending on the manufacturer and the specific product. Generally, following the manufacturer’s instructions is crucial. However, consulting with a healthcare professional is always advised, particularly for individuals with pre-existing health conditions or those taking other medications. Consistent intake and adherence to recommended dosage schedules are vital for realizing potential benefits.
Chlorella Omega-3 Supplement Brands and Key Features
| Brand | Key Features | Notes |
|---|---|---|
| Omega-3 Chlorella Plus | Combination of chlorella and fish oil, standardized for omega-3 content. | Often available in capsule form. |
| Chlorella Omega-3 Synergy | Utilizes algal oil as a source of omega-3s, potentially better for vegetarians/vegans. May include additional vitamins or minerals. | Typically in tablet or capsule form. |
| Superfood Omega-3 Chlorella | Focuses on a high chlorella content alongside a specific omega-3 source, like krill oil. | Look for details on the percentage of chlorella and omega-3s per serving. |
| Advanced Chlorella Omega-3 Complex | Formulated with chlorella and a blend of omega-3 sources, potentially including flaxseed oil or other plant-based sources. | May contain added antioxidants or digestive enzymes. |
This table provides a general overview. Always refer to the product labels for specific details regarding dosage, ingredients, and potential allergens.
Potential Interactions and Considerations

While chlorella and omega-3s are generally considered safe, potential interactions with other supplements or medications, as well as specific risks and considerations for certain individuals, should be addressed. Understanding these factors can help ensure safe and effective supplementation.Careful consideration of potential interactions is crucial for optimizing the benefits and minimizing any adverse effects of chlorella and omega-3 supplementation. This section explores these considerations in detail, emphasizing the importance of consulting with a healthcare professional before starting any new supplement regimen.
Potential Interactions with Other Supplements
Certain supplements can interact with chlorella or omega-3s, potentially altering their absorption or effectiveness. For example, chlorella may interact with medications that affect the liver or kidneys. Some individuals take iron supplements, and these supplements can affect the absorption of chlorella, requiring careful monitoring. Similarly, the use of certain herbs or supplements might affect omega-3 absorption or metabolism.
Potential Interactions with Medications
Some medications may interact with chlorella or omega-3s, either reducing their effectiveness or increasing the risk of side effects. This is particularly important for individuals taking blood thinners or medications that affect blood sugar levels. Consult with a doctor before combining chlorella or omega-3 supplements with prescription or over-the-counter medications.
Potential Risks and Side Effects
Chlorella and omega-3 supplements, while generally safe, can sometimes cause mild side effects. These can include digestive issues like bloating, gas, or diarrhea, especially with high doses. In rare cases, allergic reactions or more serious side effects may occur. It is essential to monitor for any unusual symptoms and discontinue use if necessary. Always consult a healthcare professional if you experience any significant side effects.
Considerations for Individuals with Pre-existing Health Conditions
Individuals with pre-existing health conditions, such as thyroid disorders, autoimmune diseases, or kidney problems, should exercise caution when considering chlorella or omega-3 supplementation. These supplements can potentially affect existing conditions or interact with medications. It is vital to discuss the potential risks and benefits with a healthcare professional before starting supplementation. For example, individuals with autoimmune conditions might need to be cautious due to chlorella’s potential immune-modulating effects.
Chlorella superfood omega 3 is a fantastic addition to a healthy diet, packed with nutrients. While I’m not a doctor, I’ve been researching how quickly antibiotics like amoxicillin start working to fight infections, which is helpful when you’re trying to balance health and wellness with natural supplements like chlorella. You can check out this helpful resource to learn more about the time frame for amoxicillin’s effectiveness: how quickly amoxicillin starts working.
Ultimately, chlorella’s nutritional benefits are worth considering as part of a balanced approach to health and well-being.
Safe Integration into Daily Routine
A safe approach to integrating chlorella and omega-3 supplements into a daily routine involves starting with a low dose and gradually increasing it as tolerated. This gradual approach allows the body to adjust to the supplements. Monitoring for any side effects is crucial. It’s recommended to take these supplements with food to aid digestion and minimize any stomach upset.
Always follow the manufacturer’s instructions and consult a healthcare professional for personalized advice. Additionally, it’s crucial to maintain a balanced diet and lifestyle alongside supplementation.
“Consult your doctor before starting any new supplement regimen, especially if you have underlying health conditions.”
Practical Application and Recommendations
Integrating chlorella and omega-3s into a healthy diet can be a valuable addition to your wellness routine. Proper incorporation and mindful choices regarding supplements are key to maximizing benefits and minimizing potential drawbacks. This section offers practical advice on how to incorporate these nutrients, alongside a sample meal plan and tips for selecting high-quality supplements.Understanding the best ways to incorporate chlorella and omega-3s into your diet is crucial.
Careful consideration of food sources, supplement quality, and potential interactions with other medications or health conditions will lead to a more informed and effective approach to achieving your health goals.
Incorporating Chlorella and Omega-3s into Your Diet
Choosing nutrient-rich foods is essential for optimal health. Chlorella, while often consumed as a supplement, can also be incorporated into your meals. Omega-3s are abundant in fatty fish, nuts, and seeds. To ensure a balanced intake, consider these suggestions:
- Include fatty fish in your meals at least twice a week. Salmon, tuna, mackerel, and sardines are excellent sources of omega-3s. Preparing these fish using healthy cooking methods, like baking or grilling, preserves their nutritional value.
- Incorporate flaxseeds, chia seeds, and walnuts into your diet. These seeds and nuts are rich in ALA, a type of omega-3 fatty acid. Sprinkling them on salads, yogurt, or oatmeal is a simple way to add them to your meals.
- Explore chlorella-infused recipes. Some chefs and food bloggers offer creative ways to include chlorella in smoothies, soups, or even as a powder in baked goods. Researching recipes can expand your culinary horizons and introduce new flavor profiles.
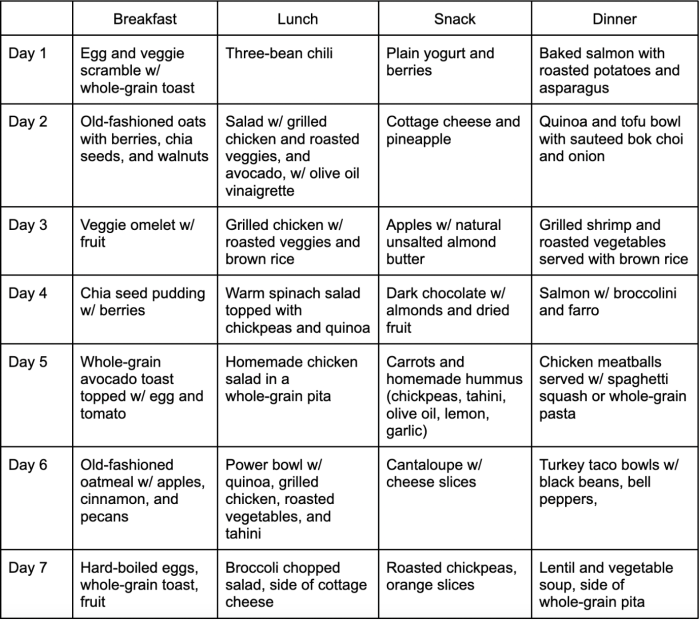
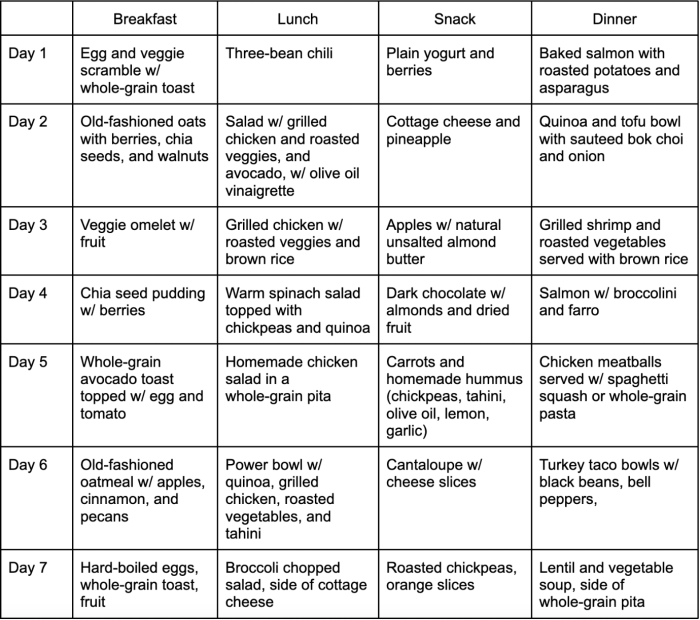
Sample Daily Meal Plan
A balanced diet, including chlorella and omega-3 sources, can significantly contribute to your overall health. This sample meal plan provides a starting point for incorporating these nutrients into your daily routine. Adjust portion sizes and ingredients to fit your individual dietary needs and preferences.
| Meal | Description | Omega-3 Source | Chlorella |
|---|---|---|---|
| Breakfast | Oatmeal with chia seeds and berries | Chia seeds | 1 teaspoon chlorella powder |
| Lunch | Salad with grilled salmon and mixed greens | Salmon | Optional: 1 teaspoon chlorella powder added to dressing |
| Dinner | Lentil soup with walnuts | Walnuts | Optional: 1 teaspoon chlorella powder added to soup |
| Snack | Handful of almonds | Almonds (contain Omega-3s) | Optional: Add 1/2 teaspoon chlorella powder to a smoothie |
Choosing High-Quality Chlorella Omega-3 Supplements
Selecting reliable chlorella and omega-3 supplements is crucial for optimal results. Consider these factors when making your purchase:
- Look for third-party certifications. Certifications like NSF International or other reputable organizations can verify the purity and quality of the supplement. These certifications provide assurance of adherence to manufacturing standards.
- Read the ingredient list carefully. Ensure the supplement contains the desired amount of chlorella and omega-3s as advertised. Avoid supplements with excessive fillers or additives.
- Check the manufacturer’s reputation and reviews. Look for companies with a strong track record and positive customer feedback. This helps ensure a reliable product.
Assessing Chlorella Product Quality and Authenticity
Verifying the quality and authenticity of chlorella products is essential. Factors to consider include:
- Source of the chlorella. Look for products sourced from reputable suppliers with a proven track record of quality control.
- Manufacturing process. Consider supplements with transparent manufacturing processes that detail the steps involved in producing the product.
- Visual inspection. Inspect the chlorella powder for its color and consistency. If the color or consistency is significantly different from the expected appearance, this might be a warning sign.
Visual Representation of Information: Chlorella Superfood Omega 3
Understanding the potential benefits of chlorella for omega-3 intake requires a clear and concise visual representation. Visual aids, like flowcharts and infographics, can effectively communicate complex information, making it easier for readers to grasp the key concepts and potential implications. This section details methods for creating such visual tools to enhance comprehension.
Flowchart Illustrating Chlorella’s Potential Omega-3 Benefits
A flowchart can visually depict the steps involved in how chlorella might contribute to omega-3 intake. This diagram can be designed with boxes and arrows, connecting different stages of the process. For instance, the flowchart would start with “Chlorella Consumption,” followed by boxes highlighting “Chlorella’s Nutritional Profile,” and “Conversion Potential.” These steps could then be linked to potential benefits such as “Increased Omega-3 Fatty Acid Levels” or “Reduced Risk of Omega-3 Deficiency.” This visual representation allows for a clear and structured overview of the process.
Infographic Summarizing Key Points on Chlorella and Omega-3s
An infographic provides a concise summary of the key aspects of chlorella and its relationship to omega-3s. This visual aid can be used to quickly communicate important information about the nutritional composition of chlorella, its potential role as a source of omega-3 fatty acids, and potential risks and benefits. The infographic can feature icons, charts, and concise text to effectively convey information.
For example, a section on “Chlorella Composition” could use a bar graph to show the presence of various nutrients, including potential omega-3 precursors.
Step-by-Step Guide to Selecting a Reputable Chlorella Supplement
Choosing a high-quality chlorella supplement requires careful consideration. Here’s a step-by-step guide to ensure you select a reputable product:
- Research and Compare Products: Look for supplements from reputable brands with a strong track record. Compare different brands and products, considering factors like the source of chlorella, manufacturing processes, and certifications. Consider the overall reputation and consumer reviews.
- Check for Certifications and Standards: Look for certifications like GMP (Good Manufacturing Practices) or other relevant industry standards. These certifications indicate that the product is manufactured to certain quality and safety guidelines. Ensure the chlorella is tested for purity and contaminants.
- Read Product Labels Carefully: Pay close attention to the product label. It should clearly list the ingredients, dosage information, and any potential allergens or warnings. Verify the specific chlorella strain or type and the total amount of chlorella per serving.
- Consider Customer Reviews and Testimonials: Examine customer reviews and testimonials from other consumers. Look for consistent feedback about the product’s quality and effectiveness. Be wary of exaggerated claims or testimonials that seem too good to be true.
- Consult with a Healthcare Professional: Before incorporating chlorella supplements into your diet, consult a healthcare professional or registered dietitian. They can provide personalized advice and guidance, especially if you have underlying health conditions.
Creating an Image Showcasing Chlorella’s Nutritional Content
To visually represent the nutritional content of chlorella, a compelling image can be created. A visually appealing image could feature a graphic representation of a chlorella tablet or powder, with the different nutrients highlighted in different colors. For instance, use different colored areas to represent protein, vitamins, minerals, and omega-3 precursors.
The image should highlight the key nutrients within chlorella, effectively showcasing its potential benefits.
A well-designed image will help consumers understand the various components present within chlorella, emphasizing its nutritional value.
Last Point
In conclusion, chlorella superfood omega 3 offers a potentially valuable addition to a balanced diet. While more research is needed, the potential benefits of incorporating chlorella into a regimen, particularly for omega-3 intake, are promising. Remember to consult with a healthcare professional before making significant dietary changes, especially if you have underlying health conditions or are taking other medications.