Reasons you have a runny nose can range from common colds to allergies. This guide delves into the various causes, symptoms, and when to seek medical attention. We’ll explore the most frequent culprits like infections and allergies, and examine less common possibilities. Understanding the reasons behind a runny nose empowers you to address it effectively.
From identifying the subtle signs of a viral infection to understanding the intricate immune response triggered by allergies, this guide provides a comprehensive overview. We’ll also explore less common causes, like nasal polyps, and highlight the importance of seeking medical advice when necessary.
Common Causes of a Runny Nose
A runny nose, medically known as rhinorrhea, is a common ailment that can be caused by various factors. Understanding these causes can help you identify the underlying issue and seek appropriate treatment. This section explores the top five most frequent reasons for a runny nose, providing detailed information on their symptoms, mechanisms, and typical durations.
Top 5 Frequent Causes of a Runny Nose
A runny nose can be a symptom of a range of conditions, from minor irritations to more serious infections. This section highlights the five most frequent causes of a runny nose, categorized by type.
Ever wondered why your nose runs? It’s usually due to a cold or allergies, but sometimes other things are at play. Interestingly, sometimes collarbone pain can be a subtle symptom of underlying conditions. If you’re experiencing persistent collarbone pain, checking out resources on causes of collarbone pain and treatment options might help. Ultimately, a runny nose is often a simple issue, but understanding potential underlying causes is important for overall well-being.
Allergies
Allergies are a common cause of a runny nose, often triggered by exposure to allergens like pollen, dust mites, pet dander, or mold. These allergens stimulate the immune system, leading to the release of histamine and other inflammatory mediators. This process results in the swelling of nasal tissues and the production of excess mucus.
- Symptoms: Typically include sneezing, itchy eyes, and a clear, watery discharge from the nose. The severity of symptoms can vary depending on the individual and the level of allergen exposure.
- Mechanism: Allergens trigger an immune response in the body. The immune system releases histamine and other inflammatory chemicals, which cause the blood vessels in the nasal passages to dilate and leak fluid. This leads to the characteristic runny nose.
- Duration: Allergic rhinitis can be seasonal or perennial. Seasonal allergies, triggered by pollen, typically last for the duration of the pollen season. Perennial allergies, triggered by indoor allergens, can persist year-round.
Viral Infections (Common Colds)
Viral infections, like the common cold, are another frequent cause of a runny nose. Viruses infect the nasal passages, causing inflammation and an increase in mucus production.
- Symptoms: Often accompanied by other symptoms such as sore throat, cough, and body aches. The nasal discharge may initially be clear but can progress to a yellowish or greenish color as the infection progresses.
- Mechanism: Viruses invade the cells lining the nasal passages, triggering an inflammatory response. The body’s immune system works to fight the infection, resulting in increased mucus production as a defense mechanism.
- Duration: The typical duration of a common cold is around 7 to 10 days. Symptoms usually peak around 3 to 5 days and gradually subside.
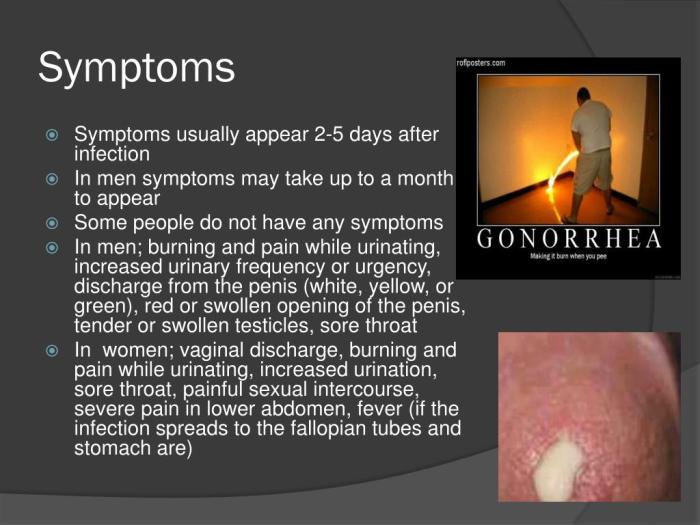
Bacterial Infections
Bacterial infections, like sinusitis, can also lead to a runny nose. Bacteria invade the sinuses and nasal passages, causing inflammation and infection.
- Symptoms: Often characterized by a thick, yellow or green nasal discharge, facial pain, and a persistent cough. Fever and fatigue can also accompany the symptoms.
- Mechanism: Bacteria multiply in the sinuses or nasal passages, causing inflammation and infection. The immune system responds to the infection, producing pus and thick mucus.
- Duration: Bacterial infections, particularly sinusitis, tend to persist longer than viral infections. Treatment is often required to resolve the infection completely. Duration can vary from a few days to several weeks.
Nasal Irritants
Exposure to irritants like smoke, dust, or chemical fumes can cause a runny nose. These irritants inflame the nasal lining, leading to increased mucus production.
- Symptoms: The discharge is usually clear or slightly white and may be accompanied by nasal itching and discomfort. The symptoms are typically less severe than those caused by allergies or infections.
- Mechanism: Irritants trigger an inflammatory response in the nasal passages, stimulating the production of mucus to flush out the irritant.
- Duration: The duration depends on the level and duration of exposure. If exposure is brief, the runny nose will likely resolve quickly once the irritant is removed. Prolonged exposure can lead to more persistent symptoms.
Dehydration
Dehydration can also cause a runny nose. A lack of sufficient fluids in the body can lead to a decrease in nasal secretions’ consistency, causing a runny nose.
- Symptoms: The runny nose associated with dehydration is often a thin, watery discharge.
- Mechanism: Dehydration disrupts the balance of fluids in the body, affecting the consistency of nasal secretions.
- Duration: The runny nose from dehydration will resolve once the body is rehydrated.
Common Causes Table
| Cause | Symptoms | Duration (approx.) |
|---|---|---|
| Allergies | Sneezing, itchy eyes, clear watery discharge | Seasonal or year-round, depending on allergen |
| Viral Infections | Sore throat, cough, body aches, initially clear then yellow/green discharge | 7-10 days |
| Bacterial Infections | Thick yellow/green discharge, facial pain, persistent cough, fever | Days to weeks |
| Nasal Irritants | Clear or slightly white discharge, nasal itching, discomfort | Variable, depends on exposure duration |
| Dehydration | Thin, watery discharge | Resolves with rehydration |
Identifying Viral Infections

A runny nose, while often a minor inconvenience, can sometimes signal a more significant health concern, particularly when accompanied by other symptoms. Understanding the different types of viral infections that can cause a runny nose is crucial for appropriate self-care and knowing when to seek medical attention. This section will delve into the world of viral infections, exploring their stages, symptoms, and potential complications.Viral infections are a common cause of a runny nose.
They’re typically less severe than bacterial infections but can still lead to discomfort and sometimes, complications. Recognizing the signs and symptoms of viral infections can help you manage them effectively and avoid unnecessary stress.
Common Viral Infections Causing a Runny Nose
Viral infections affecting the upper respiratory tract (URT) are extremely prevalent, frequently causing discomfort and temporary disruptions. Common culprits include rhinoviruses, coronaviruses, influenza viruses, and respiratory syncytial virus (RSV). Lower respiratory tract infections (LRTI) are less frequent, but more serious. These include adenoviruses and parainfluenza viruses. Distinguishing between these infections is important for appropriate treatment and management.
Stages of a Viral Infection and Runny Nose Manifestation
Viral infections typically progress through stages. The initial stage, often characterized by a runny nose, is marked by the virus’s invasion and replication within the body. The runny nose, at this stage, is often clear or slightly discolored and may be accompanied by sneezing and a sore throat. As the infection progresses, the nasal discharge might become thicker and potentially tinged with yellow or green.
This is often associated with an increase in inflammation and immune response. The recovery stage involves the body’s immune system eliminating the virus, and the runny nose typically subsides.
Comparing Viral and Bacterial Infections
While both viral and bacterial infections can cause a runny nose, their symptoms and progression differ. Viral infections often begin with a milder, more gradual onset of symptoms, with a runny nose as a key feature. Bacterial infections, on the other hand, may present with more intense symptoms that develop more quickly. The nasal discharge in bacterial infections is often thicker and more pus-like.
Additionally, bacterial infections often present with fever and more severe body aches.
A runny nose can be caused by allergies, colds, or even just a dry climate. Sometimes, though, it might be a bit more complicated. Learning how to explain skin conditions like vitiligo to others can be tricky, just like figuring out the root cause of a persistent runny nose. Understanding the different factors, like genetics or autoimmune issues, is key.
For tips on how to navigate those conversations, check out this helpful resource on explaining vitiligo to others. Ultimately, understanding the potential causes, from environmental triggers to more complex medical issues, is the best way to tackle a runny nose.
Duration of a Viral Runny Nose
The duration of a viral runny nose can vary significantly, typically ranging from a few days to two weeks. The length depends on the specific virus, the individual’s immune response, and the severity of the infection. It’s essential to monitor symptoms and seek medical advice if they persist or worsen beyond the typical duration of a viral infection.
Keeping a record of symptoms and duration helps differentiate between a viral infection and other potential causes of a runny nose.
Distinguishing from Other Causes
Other causes of a runny nose include allergies, environmental irritants, and certain medical conditions. The key to differentiating a viral infection from these other causes is the overall symptom picture. A thorough review of accompanying symptoms, like fever, body aches, and fatigue, will assist in proper diagnosis. Consulting with a healthcare professional is crucial for accurate diagnosis and appropriate management.
Viral Infections: Symptoms, Duration, and Potential Complications
| Infection | Symptoms | Duration | Potential Complications |
|---|---|---|---|
| Rhinovirus (Common Cold) | Runny nose, sneezing, sore throat, cough, mild headache | 2-14 days | Ear infections, sinus infections, bronchitis |
| Influenza (Flu) | High fever, body aches, headache, fatigue, cough, runny nose | 7-10 days | Pneumonia, bronchitis, dehydration |
| Coronavirus (COVID-19) | Fever, cough, fatigue, shortness of breath, runny nose | 2-14 days (variable) | Severe pneumonia, acute respiratory distress syndrome (ARDS) |
| RSV (Respiratory Syncytial Virus) | Runny nose, cough, wheezing, shortness of breath (especially in infants and young children) | 5-10 days | Bronchiolitis, pneumonia |
Allergies and a Runny Nose: Reasons You Have A Runny Nose
A runny nose, a common ailment, can have various underlying causes. While viral infections are a frequent culprit, allergies play a significant role in this condition. Understanding the different types of allergies and the immune responses they trigger is crucial for effective management and treatment.Allergic reactions, specifically allergic rhinitis, are an exaggerated immune response to harmless substances called allergens.
These allergens, like pollen or pet dander, trigger the release of histamine and other inflammatory mediators, leading to the characteristic symptoms of a runny nose, sneezing, and itchy eyes. This immune response is mediated by specialized immune cells, including mast cells and basophils. The inflammatory cascade results in the symptoms we experience.
Types of Allergic Reactions
Allergic rhinitis, often referred to as hay fever, is a common type of allergic reaction involving the nasal passages. Different allergens can trigger these reactions. Identifying the specific allergens is crucial for personalized treatment plans.
Common Allergens
A wide array of substances can act as allergens. Some of the most common culprits include pollen from various plants, especially grasses, trees, and weeds. Dust mites, tiny creatures found in house dust, are also frequent offenders. Pet dander, tiny flakes of skin shed by pets, can trigger reactions in susceptible individuals. Mold spores, present in damp environments, can also be potent allergens.
Immune Response in Allergic Reactions
The immune system’s response to allergens in allergic individuals is distinct from its response in healthy individuals. When an allergen encounters a sensitized individual, the body’s immune system mistakenly identifies it as a threat. Specialized immune cells, like mast cells, release inflammatory mediators, including histamine. This release triggers the characteristic symptoms associated with allergic reactions, such as nasal congestion, sneezing, and itching.
Environmental Factors and Allergic Rhinitis
Environmental factors significantly influence the severity of allergic rhinitis. High pollen counts during specific times of the year, for example, can exacerbate symptoms in susceptible individuals. Indoor allergens, such as dust mites, can be more prevalent in poorly maintained or humid environments. Exposure to allergens in these environments leads to more frequent and intense reactions.
Allergy Types, Common Allergens, and Symptoms
| Allergy Type | Common Allergens | Symptoms |
|---|---|---|
| Pollen Allergies (Seasonal Allergies) | Tree pollen, grass pollen, weed pollen | Runny nose, sneezing, itchy eyes, congestion, and sometimes a sore throat. |
| Dust Mite Allergies | Dust mites, their feces and shed skins | Runny nose, sneezing, congestion, and itchy eyes. Symptoms are often worse at night or in dusty environments. |
| Pet Dander Allergies | Pet dander (from cats, dogs, and other animals) | Runny nose, sneezing, congestion, and itchy eyes. Symptoms may worsen upon contact with the pet. |
| Mold Allergies | Mold spores | Runny nose, sneezing, congestion, and itchy eyes. Symptoms are often worse in damp environments. |
Other Potential Causes
A runny nose, while often associated with common colds or allergies, can stem from various other factors. Understanding these less common causes can aid in proper diagnosis and treatment. These causes can range from benign conditions like nasal polyps to more serious underlying medical issues. It’s crucial to distinguish between these less common causes and more prevalent ones to ensure appropriate medical intervention.Identifying the root cause of a runny nose is vital for effective management and treatment.
A thorough evaluation by a healthcare professional is essential for accurate diagnosis and tailored care.
Nasal Polyps
Nasal polyps are benign growths that develop inside the nasal passages. These growths can cause a persistent runny nose, often accompanied by nasal congestion and a feeling of fullness in the head. The underlying mechanism involves chronic inflammation within the nasal tissues, leading to the development of these growths. Symptoms frequently include difficulty breathing through the nose, a persistent stuffy nose, and facial pressure.
Certain Medications
Certain medications can trigger a runny nose as a side effect. Some medications, such as certain blood pressure drugs, antihistamines, and decongestants, can cause a runny nose as a side effect. The mechanism behind this involves the impact of these drugs on the delicate lining of the nasal passages. The specific medication and its dosage can influence the duration and severity of the runny nose.
Foreign Bodies
A less common cause of a runny nose is the presence of a foreign body lodged within the nasal passages. This can be anything from small objects like beads or pieces of food to insects. The body’s natural reaction to the presence of a foreign body includes producing mucus to try to flush it out. Symptoms can include a persistent runny nose, unilateral nasal discharge, and potential discomfort or pain.
The duration of the runny nose depends on when the object is removed, ranging from hours to days.
Hormonal Changes
Hormonal changes, particularly during pregnancy or menopause, can affect the nasal lining, potentially leading to a runny nose. The fluctuating hormone levels can cause increased mucus production and nasal congestion. Symptoms often include a watery discharge and nasal congestion, which can vary in severity. The duration of the runny nose depends on the hormonal fluctuation and its resolution.
Tumors
Nasal tumors, while rare, can manifest with a runny nose. Tumors can cause a persistent runny nose, often accompanied by other symptoms like facial pain or headaches. The specific type of tumor and its location will influence the symptoms and duration. The duration of the runny nose can vary greatly depending on the tumor’s size, type, and growth rate.
When to Seek Medical Attention

A runny nose is a common ailment, often resolving on its own.
However, certain symptoms and situations necessitate immediate medical attention to rule out potentially serious underlying conditions. Understanding these warning signs is crucial for ensuring prompt and appropriate care.While most cases of a runny nose are benign and resolve within a week or two, some indicate a more serious problem requiring medical intervention. It’s important to recognize the subtle differences that might signal a need for professional evaluation.
This section details the situations where a runny nose warrants immediate medical attention and explains the signs and symptoms that might indicate a serious underlying condition.
Serious Symptoms Requiring Immediate Medical Attention
A persistent runny nose accompanied by other concerning symptoms necessitates immediate medical evaluation. These symptoms could signal a more severe infection or condition that requires prompt treatment.
- High fever (100.4°F or higher): A high fever, particularly when accompanied by a runny nose, can indicate an infection that needs prompt medical attention. Examples include bacterial infections or severe viral illnesses like influenza.
- Severe headache or facial pain: Headaches or facial pain associated with a runny nose might suggest complications from a sinus infection or other conditions.
- Difficulty breathing or shortness of breath: Difficulty breathing, whether accompanied by a runny nose or not, requires immediate medical evaluation. It could indicate a more serious respiratory condition or allergic reaction.
- Presence of blood in the nasal discharge: Blood in the nasal discharge, even a small amount, warrants immediate medical attention to determine the cause. This could be a sign of a serious injury or an underlying medical condition.
- Persistent nasal blockage that doesn’t respond to home remedies: A persistent nasal blockage that doesn’t improve with saline nasal sprays or other home treatments should prompt a visit to the doctor.
- New onset of neurological symptoms: Sudden onset of symptoms like confusion, seizures, or weakness, especially when combined with a runny nose, demand immediate medical attention. These could signal a serious neurological issue.
Reasons to See a Doctor About a Runny Nose, Reasons you have a runny nose
There are several reasons why you should consult a medical professional about a runny nose, even if it doesn’t involve severe symptoms.
- Runny nose lasting longer than 10 days: A runny nose that persists for more than 10 days without improvement might indicate a bacterial infection or other underlying cause.
- Runny nose accompanied by a persistent cough: A runny nose accompanied by a cough that doesn’t subside might signal a respiratory infection.
- Runny nose associated with difficulty swallowing: If a runny nose is accompanied by difficulty swallowing, it could indicate a throat or nasal infection requiring medical attention.
- Runny nose and difficulty smelling or tasting: Loss of smell or taste associated with a runny nose could indicate a sinus infection or other conditions affecting the nasal passages.
- Runny nose with unexplained fatigue and body aches: Unexplained fatigue and body aches along with a runny nose might signal a more serious illness.
Examples of Scenarios Requiring Medical Intervention
Certain scenarios involving a runny nose highlight the importance of prompt medical attention.
- A child with a runny nose, high fever, and difficulty breathing needs immediate medical attention. This is a critical scenario demanding swift action.
- An adult experiencing a runny nose, severe headache, and facial pain should seek immediate medical evaluation.
- A person with a runny nose and blood in their nasal discharge should seek immediate medical attention to determine the cause.
Decision-Making Flowchart for Seeking Medical Care
This flowchart illustrates a decision-making process for when to seek medical care for a runny nose. It’s not exhaustive, but provides a general guide.
Ugh, a runny nose is the worst! It can be caused by allergies, colds, or even just dry air. Sometimes, you might be tempted to reach for a vitamin C boost, like Emergen-C, wondering if it helps. While the vitamin C in Emergen-C might give you a little pep, does Emergen C work to actually treat a runny nose?
The truth is, it likely won’t cure the underlying cause, but it might help you feel a bit better overall. So, if you’re looking for a quick fix for a runny nose, try looking into the root cause instead.
| Symptom | Action |
|---|---|
| Mild runny nose, lasting a few days, no other symptoms | Monitor at home, use home remedies. |
| Runny nose with fever, headache, or difficulty breathing | Seek immediate medical attention. |
| Runny nose lasting longer than 10 days, no improvement with home remedies | Consult a doctor. |
| Runny nose with blood, loss of smell/taste, or neurological symptoms | Seek immediate medical attention. |
Home Remedies and Self-Care
A runny nose can be incredibly bothersome, impacting daily activities and comfort. While seeking medical attention for severe or persistent symptoms is crucial, various home remedies can offer symptom relief and provide comfort. These methods, when used appropriately, can complement medical advice and help manage the discomfort of a runny nose.
Symptom Relief Strategies
Effective home remedies for a runny nose often focus on alleviating congestion, promoting drainage, and soothing irritated tissues. These approaches, when used judiciously, can ease discomfort and improve overall well-being.
Saline Nasal Sprays
Saline nasal sprays are a safe and effective way to rinse nasal passages and loosen congestion. The gentle saline solution helps clear mucus and irritants, promoting a sense of relief. Using a saline spray several times a day can significantly aid in managing a runny nose. Proper use involves carefully spraying the solution into each nostril, ensuring the solution reaches the affected areas.
A noticeable improvement in nasal drainage is often observed with regular use.
Humidifiers
Adding moisture to the air can significantly reduce nasal dryness and congestion. Humidifiers help to keep nasal passages moist, which can lessen the irritation and discomfort of a runny nose. Using a humidifier can create a more comfortable environment, especially during dry seasons or in dry climates. Carefully maintain the humidifier by regularly cleaning it to prevent the growth of mold or bacteria.
Rest and Hydration
Adequate rest and hydration are crucial for the body to fight off infection and recover from a runny nose. Getting enough sleep allows the body to repair itself, while drinking plenty of fluids helps thin mucus and promotes proper hydration. Aim for at least eight hours of sleep per night and drink plenty of water, herbal teas, or clear broths.
Warm Compresses
Applying warm compresses to the forehead or sinuses can help to soothe discomfort and promote drainage. The warmth helps to open up the nasal passages, allowing for easier mucus flow. Using a warm, damp cloth or a warm compress can bring comfort and relief. However, avoid using excessively hot compresses to prevent burns.
Comparison of Remedies
Saline nasal sprays are generally considered a safe and effective first-line treatment for nasal congestion. Humidifiers are beneficial for maintaining nasal moisture and reducing dryness, which is often associated with a runny nose. Adequate rest and hydration are crucial for overall recovery, but they do not directly address the runny nose itself. Warm compresses offer soothing relief and can help with drainage.
The effectiveness of each remedy can vary based on individual experiences and the cause of the runny nose.
Important Considerations
- Saline Nasal Sprays: A safe and effective way to clear nasal passages. Use as directed. Do not use excessively, as this can irritate the nasal passages.
- Humidifiers: Help to keep nasal passages moist. Clean regularly to prevent mold or bacterial growth. Ensure the humidity level is not too high, which can lead to other issues.
- Rest and Hydration: Essential for overall recovery. Adequate sleep and fluids are crucial for the body to heal.
- Warm Compresses: Provide soothing relief and may promote drainage. Avoid excessively hot compresses to prevent burns.
Ultimate Conclusion
In conclusion, a runny nose, while often a minor inconvenience, can stem from various underlying causes. By understanding the common triggers, like allergies and infections, as well as the less frequent possibilities, you can better manage your symptoms and make informed decisions about your health. This guide has provided insights into the complexities of a runny nose, equipping you with knowledge to navigate this common ailment.
Remember, when in doubt, consult a healthcare professional.