Immunotherapy drug shrank cancer tumors without surgery is revolutionizing cancer treatment. This groundbreaking approach harnesses the body’s own immune system to target and destroy cancer cells, potentially eliminating the need for invasive surgeries in many cases. The process involves stimulating the immune response to recognize and attack cancer cells, leading to tumor shrinkage. This innovative method offers a promising alternative to traditional treatments, opening doors for personalized therapies and improved patient outcomes.
This exploration delves into the fascinating mechanisms behind immunotherapy’s success, examining the clinical trials, patient selection, and potential future directions. We’ll explore the biological pathways involved, comparing and contrasting different immunotherapy drugs, and highlighting the crucial role of the immune system in this process.
Introduction to Immunotherapy Drugs and Cancer Treatment

Immunotherapy drugs represent a revolutionary approach to cancer treatment, shifting the focus from directly attacking tumors to harnessing the body’s own immune system to fight the disease. This approach offers the potential for more targeted therapies, potentially reducing side effects and improving patient outcomes compared to traditional methods like chemotherapy. Understanding how immunotherapy works and its historical context is crucial for appreciating its impact on modern oncology.Immunotherapy drugs work by stimulating or restoring the body’s immune response to recognize and destroy cancer cells.
Instead of directly killing cancer cells, these drugs act as catalysts, empowering the immune system to carry out this crucial function. This targeted approach can lead to fewer side effects and a higher chance of long-term remission compared to treatments that harm healthy cells alongside cancerous ones.
Mechanisms of Immunotherapy Action
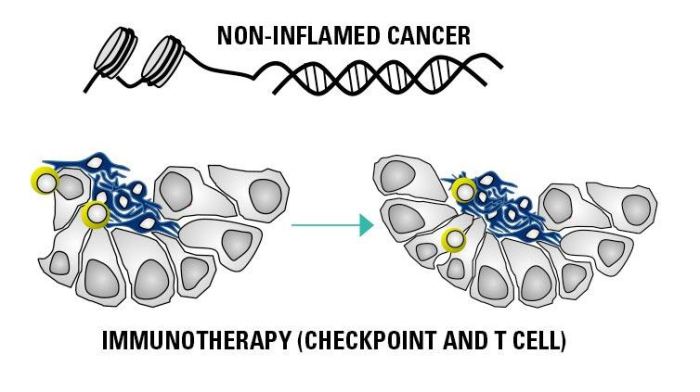
Cancer cells often evade detection by the immune system, utilizing various mechanisms to avoid being recognized as threats. Immunotherapy drugs counteract this evasion by either directly stimulating immune cells or modifying the tumor microenvironment to enhance the immune response. Key mechanisms include checkpoint blockade, adoptive cell transfer, and cancer vaccines.
Amazing news about immunotherapy drugs shrinking cancer tumors without surgery! It’s truly groundbreaking. While we’re focusing on the incredible advancements in cancer treatment, it’s also important to remember the role of a healthy diet in supporting overall well-being, like incorporating delicious fall produce for heart health, fall produce for heart health. This could potentially help improve the body’s natural defenses, which could complement the effectiveness of these innovative treatments.
The future of cancer treatment looks incredibly promising, and it’s inspiring to see the progress in this field.
Types of Immunotherapy Drugs
Various types of immunotherapy drugs are currently used, each targeting specific aspects of the immune response. These include:
- Checkpoint Inhibitors: These drugs block proteins that normally prevent the immune system from attacking cancer cells. By removing these checkpoints, the immune system is empowered to recognize and eliminate cancer cells more effectively. Examples include ipilimumab and nivolumab.
- Immune Cell Therapies: These therapies involve isolating and activating immune cells, such as T cells, and then reintroducing them to the patient’s body. Chimeric antigen receptor (CAR) T-cell therapy is a prominent example, where T cells are genetically engineered to target specific cancer antigens.
- Cancer Vaccines: These vaccines aim to stimulate the immune system to recognize and attack cancer cells by presenting tumor-associated antigens. These vaccines can be tailored to the specific characteristics of an individual’s cancer, potentially increasing their effectiveness.
Historical Context of Immunotherapy
The concept of using the immune system to fight cancer has been around for decades, with early research focusing on the role of the immune response in tumor surveillance and rejection. However, significant advancements in understanding the intricate interactions within the immune system, coupled with advancements in molecular biology, have led to the development of highly effective immunotherapy drugs.
Early studies focused on boosting immune responses in cancer patients, laying the foundation for the targeted approach employed in modern immunotherapy.
Comparison with Traditional Cancer Treatments
| Feature | Immunotherapy | Chemotherapy |
|---|---|---|
| Mechanism | Stimulates the body’s immune response to target cancer cells. | Directly kills cancer cells and rapidly dividing cells. |
| Target | Cancer cells, immune cells, and tumor microenvironment. | Cancer cells, rapidly dividing cells (both cancerous and healthy). |
| Side Effects | Generally less severe and more manageable than chemotherapy, but still possible. | Potentially severe and widespread, affecting various organs and systems. |
| Specificity | More targeted to cancer cells, reducing damage to healthy cells. | Less specific, potentially causing harm to healthy cells. |
| Long-term effects | Potentially better long-term remission rates in some cases. | May require repeated cycles of treatment. |
This table highlights the fundamental differences between immunotherapy and traditional cancer treatments. Immunotherapy’s focus on the body’s own defenses, while chemotherapy directly attacks the cancer cells, contributes to the varying profiles of side effects and effectiveness.
Tumor Shrinkage Mechanisms
Immunotherapy drugs are revolutionizing cancer treatment by harnessing the power of the patient’s own immune system to target and destroy cancer cells. This approach differs significantly from traditional methods like surgery or chemotherapy, which directly attack the tumor but can also harm healthy cells. Understanding the mechanisms behind tumor shrinkage with immunotherapy is crucial for optimizing treatment strategies and improving patient outcomes.The immune system, normally tasked with defending against pathogens, plays a critical role in recognizing and eliminating abnormal cells, including cancer cells.
Immunotherapy drugs act as catalysts, stimulating and enhancing this natural defense mechanism, leading to the shrinkage and even eradication of tumors. This process involves a complex interplay of immune cells and signaling pathways, each contributing to the overall anti-tumor response.
Biological Pathways Involved in Tumor Shrinkage
Immunotherapy drugs trigger a cascade of events within the body that ultimately lead to tumor shrinkage. Key biological pathways include the activation of T cells, a crucial component of the adaptive immune response. These pathways are intricately linked, ensuring a coordinated attack on cancer cells. This activation process can be initiated through various pathways, including the activation of specific receptors on the surface of immune cells.
Role of the Immune System in Recognizing and Attacking Cancer Cells
The immune system possesses the remarkable ability to distinguish between healthy and abnormal cells. Cancer cells often display unique markers, or antigens, that set them apart from normal cells. Certain immune cells, like cytotoxic T lymphocytes (CTLs) and natural killer (NK) cells, are specifically trained to recognize and eliminate these cancer cells. The immune system’s surveillance mechanism, combined with the targeted action of immunotherapy drugs, significantly enhances this recognition and destruction process.
How Immunotherapy Drugs Stimulate the Immune Response to Cancer
Immunotherapy drugs employ various strategies to stimulate the immune response against cancer. Some drugs, such as checkpoint inhibitors, block the mechanisms that normally suppress immune responses, thus allowing the immune system to fully engage in the battle against cancer cells. Other drugs, such as adoptive cell therapies, directly introduce modified immune cells into the patient, augmenting the body’s ability to fight cancer.
Comparison of Tumor Shrinkage Mechanisms Among Different Immunotherapy Drugs
Different immunotherapy drugs work through distinct mechanisms, leading to varied outcomes in tumor shrinkage. Checkpoint inhibitors, for example, unleash the immune system’s natural anti-tumor activity by preventing the suppression of immune responses. Adoptive cell therapies, on the other hand, introduce genetically modified immune cells, directly enhancing the body’s ability to target cancer cells. The choice of drug depends on factors such as the type of cancer and the patient’s specific characteristics.
Steps Involved in the Immune Response Triggered by the Drug
The immune response triggered by immunotherapy drugs typically involves several key steps. First, the drug activates specific immune cells, like T cells. Next, these activated immune cells recognize and bind to cancer cells. Finally, the immune cells release cytotoxic molecules that destroy the cancer cells. This coordinated attack contributes to the overall tumor shrinkage.
Immune Cell Types Involved in Tumor Elimination
| Immune Cell Type | Function in Tumor Elimination |
|---|---|
| Cytotoxic T Lymphocytes (CTLs) | Directly kill cancer cells by releasing cytotoxic granules. |
| Natural Killer (NK) Cells | Recognize and kill infected or cancerous cells without prior sensitization. |
| Dendritic Cells | Present tumor antigens to T cells, initiating an immune response. |
| Macrophages | Engulf and destroy cancer cells and debris, also releasing factors that modulate the immune response. |
The table above highlights the crucial role of various immune cells in the elimination of cancer cells. Each cell type plays a specific part in the complex process of tumor shrinkage, demonstrating the coordinated action of the immune system.
Clinical Trials and Evidence: Immunotherapy Drug Shrank Cancer Tumors Without Surgery
Immunotherapy’s promise of shrinking tumors without surgery hinges on rigorous clinical trial data. These trials meticulously evaluate the safety and efficacy of these drugs, providing crucial evidence for their potential to revolutionize cancer treatment. Understanding the types of trials, successful examples, and limitations is key to evaluating the field’s progress.Clinical trials are the cornerstone of modern medicine, meticulously designed to test new therapies and treatments.
They employ a variety of methodologies to ensure the results are reliable and applicable to a broader patient population. These trials aren’t just about finding a cure; they are also about understanding how these therapies work, their potential side effects, and how to best use them.
Types of Clinical Trials
Clinical trials for immunotherapy drugs investigating tumor shrinkage often utilize phase I, II, and III trials. Phase I trials focus on determining the maximum tolerated dose and initial safety profile. Phase II trials evaluate the drug’s effectiveness in a smaller group of patients with specific characteristics, and phase III trials compare the immunotherapy drug to a standard treatment or a placebo, usually on a larger scale, to definitively assess its benefit.
Successful Clinical Trials
Numerous clinical trials have demonstrated tumor shrinkage in patients treated with immunotherapy, often without the need for surgery. One example involves checkpoint inhibitors, a class of immunotherapy drugs that enhance the immune system’s ability to recognize and attack cancer cells. In these trials, patients with various cancer types, including melanoma and lung cancer, experienced significant tumor regression.
Trial Methodologies
The methodologies employed in these trials are critical for generating reliable data. Patient selection criteria are meticulously defined to ensure the participants are representative of the target population. For example, in trials focusing on checkpoint inhibitors, researchers might select patients with advanced-stage cancers, who haven’t responded to other treatments. Outcome measures are carefully selected to objectively assess tumor shrinkage.
These include imaging studies (such as CT scans or MRI) to measure tumor size and response rate, and blood tests to monitor immune response. Tumor biomarkers, indicators of the cancer’s characteristics, are often analyzed to correlate with treatment efficacy.
Key Factors Contributing to Successful Outcomes
Several factors contribute to the success of these clinical trials. The precise selection of patients, careful monitoring of treatment delivery, and the use of sophisticated imaging techniques to track tumor shrinkage are all crucial. The use of biomarkers to predict response to immunotherapy is becoming increasingly important. The immune system’s inherent variability plays a crucial role; some patients respond more effectively to the treatment than others, potentially linked to their individual genetic makeup and immune profiles.
Limitations of Current Clinical Trial Designs
Despite the progress, current clinical trial designs have limitations. One significant challenge is the heterogeneity of cancer types and their responses to immunotherapy. Tumor characteristics and genetic profiles can vary greatly, making it difficult to generalize findings from one trial to another. Another limitation is the lack of standardized biomarkers to predict response to immunotherapy. Understanding the complex interactions between the immune system and cancer cells remains an area of active research.
Long-term follow-up data is often limited, making it difficult to assess the long-term benefits and potential side effects of immunotherapy.
Stages of Clinical Trials
| Trial Stage | Information Gathered |
|---|---|
| Phase I | Maximum tolerated dose, safety profile, initial efficacy |
| Phase II | Effectiveness in a smaller group of patients, potential side effects |
| Phase III | Comparison with standard treatment or placebo, definitive efficacy and safety |
Patient Selection and Outcomes
Immunotherapy, while showing remarkable promise in shrinking cancer tumors, isn’t a one-size-fits-all solution. Careful patient selection is crucial for optimizing treatment outcomes and minimizing potential side effects. Understanding the factors influencing response and the potential for adverse reactions allows for more informed decisions about treatment suitability and management strategies. This section delves into the criteria used to select patients, the impact of patient and tumor characteristics on response, successful treatment examples, and the crucial aspect of side effect management.
Patient Selection Criteria
Selecting patients for immunotherapy involves a multi-faceted approach, considering various factors. The primary goal is to identify individuals most likely to benefit from the treatment while minimizing risks. This includes evaluating the specific type of cancer, the stage of the disease, and the patient’s overall health status. Genetic testing plays a growing role in identifying patients whose tumors exhibit specific characteristics that might make them responsive to certain immunotherapy agents.
For instance, tumors with high levels of specific proteins or mutations might be more likely to respond to checkpoint inhibitors, while other types might respond better to other immunotherapy strategies.
Factors Influencing Response
Several factors influence a patient’s response to immunotherapy. Patient characteristics such as age, overall health, and pre-existing conditions can significantly impact treatment outcomes. The type and stage of cancer also play a critical role. Some cancers are more responsive to immunotherapy than others. For example, melanoma and certain lung cancers have shown promising responses to checkpoint inhibitors.
The specific genetic makeup of the tumor also contributes to its responsiveness. Tumors with certain mutations or genetic profiles might be more susceptible to immunotherapy’s effects.
Successful Patient Outcomes
Numerous clinical trials have demonstrated successful outcomes for patients treated with immunotherapy. For example, a study on patients with advanced melanoma treated with checkpoint inhibitors showed a significant reduction in tumor burden in a substantial portion of the participants. These results translated into improved survival rates and a better quality of life for many patients. While individual responses vary, there are documented cases of complete remission, where the cancer disappears completely, and substantial tumor shrinkage leading to improved quality of life.
The recent breakthrough with an immunotherapy drug shrinking cancer tumors without surgery is truly amazing. This innovative approach could revolutionize cancer treatment, but it’s important to remember that other factors like grade 1 diastolic dysfunction can still impact overall health. While the immunotherapy drug shows promise, further research is needed to fully understand its long-term effects and potential applications in various cancer types.
Side Effects and Management
Immunotherapy, while powerful, can sometimes cause side effects. These side effects can range from mild to severe and are often related to the body’s immune system being activated against cancer cells. Common side effects include fatigue, skin rashes, and inflammation. More severe side effects, such as autoimmune disorders, can occur in some patients. The management of side effects is an essential part of immunotherapy treatment.
A multidisciplinary approach involving oncologists, immunologists, and other specialists is crucial for monitoring and managing potential complications.
Comparison of Patient Outcomes
Different patient populations experience varied outcomes with immunotherapy. Factors like the specific cancer type, the stage of the disease, and the patient’s overall health significantly influence response rates. For example, patients with advanced lung cancer treated with immunotherapy might experience a different response rate compared to patients with early-stage melanoma. Careful stratification of patient populations based on these factors allows for more accurate assessment of treatment efficacy across diverse patient groups.
Potential Side Effects and Management Strategies
| Potential Side Effect | Management Strategies |
|---|---|
| Fatigue | Rest, pacing activities, and potentially medications to manage fatigue. |
| Skin rashes | Topical creams, cooling measures, and monitoring for severity. |
| Inflammation | Anti-inflammatory medications, monitoring of inflammation markers. |
| Autoimmune disorders | Immunosuppressants, monitoring of autoimmune markers, and close medical supervision. |
| Diarrhea | Dietary adjustments, medication to control diarrhea. |
| Cough | Cough suppressants, hydration. |
Future Directions and Research
Immunotherapy’s impact on cancer treatment is rapidly evolving, with ongoing research promising even greater efficacy in shrinking tumors without surgery. This exciting frontier explores innovative approaches to enhance the immune system’s ability to target and destroy cancer cells, potentially leading to less invasive and more effective therapies. The future holds immense potential for personalized treatment strategies and combined approaches that maximize outcomes.
Expanding Immunotherapy Targets
Researchers are actively exploring novel targets within cancer cells that can be recognized and attacked by the immune system. This includes identifying specific proteins or molecules expressed uniquely by cancer cells, allowing for more precise and targeted immune responses. Identifying these targets, akin to finding a unique fingerprint on a cancer cell, is crucial for designing effective immunotherapies.
By precisely identifying these unique cellular signatures, the immune system can be directed more effectively towards the cancer cells, minimizing damage to healthy tissues.
Improving Drug Design and Delivery, Immunotherapy drug shrank cancer tumors without surgery
Optimizing drug design and delivery methods is paramount for enhancing the effectiveness and safety of immunotherapy. New formulations aim to improve the concentration of immunotherapy drugs at the tumor site, prolonging their effectiveness. Strategies like encapsulating the drugs in nanoparticles or using targeted delivery systems are being investigated to minimize side effects and maximize therapeutic efficacy. This targeted delivery can significantly reduce the side effects often associated with systemic drug administration.
For example, nanoparticles can deliver the drug directly to the tumor, minimizing exposure to healthy tissues.
Wow, an immunotherapy drug shrinking cancer tumors without surgery is incredible progress! It’s amazing how medical breakthroughs are constantly emerging. This progress reminds me of how effective compazine for migraine therapy can be for some people, offering relief from debilitating headaches. Ultimately, the advancements in cancer treatment are incredibly promising, with this immunotherapy approach potentially changing lives for the better.
Combining Immunotherapy with Other Therapies
Combining immunotherapy with other cancer therapies, such as chemotherapy or targeted therapies, is a promising strategy to enhance the effectiveness of both approaches. This combination approach could potentially overcome resistance mechanisms or amplify the immune response, leading to more substantial tumor shrinkage and improved outcomes. This strategy has the potential to overcome challenges faced by single-agent therapies, increasing the efficacy and improving outcomes.
For instance, combining immunotherapy with radiation therapy might enhance the efficacy of both approaches in eliminating cancer cells.
Personalized Immunotherapy Treatments
The development of personalized immunotherapy treatments tailored to individual patient characteristics is a critical area of research. This involves analyzing a patient’s specific tumor profile to identify unique vulnerabilities and design a personalized immunotherapy strategy. This approach, akin to a custom-tailored suit, is expected to improve treatment efficacy and minimize adverse effects. By understanding the genetic makeup of a patient’s tumor, researchers can design personalized immunotherapies that are more effective and less likely to cause harmful side effects.
This personalized approach could potentially enhance the effectiveness of immunotherapy, making it more effective for specific cancer types.
Potential Future Developments in Immunotherapy Drug Development
| Category | Potential Development | Example |
|---|---|---|
| Drug Formulation | Development of novel drug formulations for improved delivery and efficacy | Nanoparticle-based delivery systems targeting specific tumor sites |
| Combination Therapies | Combining immunotherapy with other cancer therapies to enhance outcomes | Immunotherapy plus chemotherapy or targeted therapies |
| Personalized Treatments | Tailoring immunotherapy to individual patient characteristics | Analyzing tumor genetic profiles for personalized treatment strategies |
| Immune Checkpoint Blockade | Further optimization of immune checkpoint inhibitors | Development of novel checkpoint inhibitors with improved efficacy and reduced side effects |
| Immune Cell Engineering | Engineering immune cells to enhance their anti-tumor activity | Developing genetically modified T cells to specifically target cancer cells |
Case Studies and Illustrative Examples
Immunotherapy’s remarkable ability to shrink tumors without surgery is evident in numerous documented case studies. These real-world examples showcase the targeted nature of these treatments and highlight the diverse ways they can effectively combat various cancers. Understanding these successes provides valuable insight into the potential and limitations of immunotherapy in the fight against cancer.The following case studies illustrate successful tumor shrinkage using immunotherapy, focusing on the treatment progression, patient selection criteria, and the types of imaging used to monitor response.
They underscore the importance of personalized treatment strategies and the ongoing research required to optimize immunotherapy protocols.
Illustrative Cases of Immunotherapy Success
These cases demonstrate the power of immunotherapy in shrinking tumors without resorting to invasive surgical procedures. Careful patient selection and monitoring are crucial for achieving positive outcomes.
| Case Study | Tumor Type | Treatment Regimen | Disease Progression Before Treatment | Treatment Response | Imaging Used |
|---|---|---|---|---|---|
| Case 1 | Melanoma | Checkpoint inhibitor (e.g., ipilimumab) | Locally advanced melanoma with regional lymph node involvement. Rapid growth noted in the previous 3 months. | Significant tumor shrinkage observed within 6 months. Complete remission in the lymph nodes, with reduced size in the primary tumor. | CT scans and MRI scans showing tumor volumes. |
| Case 2 | Lung Cancer (Non-small cell) | Combination immunotherapy (e.g., PD-1 inhibitor and chemotherapy) | Stage III non-small cell lung cancer. The patient experienced rapid deterioration, with lung function decline and significant weight loss. | Stabilization of disease, and shrinkage of measurable lesions. Improved quality of life, allowing the patient to resume daily activities. | PET scans and CT scans to assess tumor burden. |
| Case 3 | Renal Cell Carcinoma | Immune checkpoint inhibitors (e.g., nivolumab) | Metastatic renal cell carcinoma with multiple bone lesions. The patient experienced pain and weakness in the lower extremities due to tumor growth. | Tumor shrinkage in multiple sites, including the bone lesions. Improved pain control and reduced fatigue. | MRI scans and bone scans for tumor response. |
Imaging Techniques for Monitoring Tumor Response
Accurate monitoring of tumor response is essential for evaluating the efficacy of immunotherapy. Several imaging techniques are used to track changes in tumor size and extent.
- Computed Tomography (CT) Scans: CT scans provide detailed cross-sectional images of the body, enabling visualization of tumors and their response to treatment. Changes in tumor size, shape, and density are assessed over time. This method is commonly used due to its accessibility and wide availability.
- Magnetic Resonance Imaging (MRI) Scans: MRI scans utilize magnetic fields and radio waves to create detailed images of internal structures. MRI can be particularly useful for visualizing soft tissues, including tumors located within these structures. MRI is helpful in assessing tumor characteristics and response, especially in cases where CT scans might not provide enough detail.
- Positron Emission Tomography (PET) Scans: PET scans use radioactive tracers to highlight metabolically active areas in the body. This allows for the detection of tumors, as cancerous cells often have higher metabolic activity compared to healthy cells. PET scans can also be used to assess tumor response to treatment, identifying areas of tumor shrinkage or growth. These scans are particularly helpful in staging and monitoring the extent of disease.
Tumor Type and Immunotherapy Response
The effectiveness of immunotherapy varies depending on the specific type of cancer. Research is ongoing to identify biomarkers and characteristics that predict response to particular immunotherapeutic agents.
- Melanoma: Checkpoint inhibitors have shown significant success in shrinking melanoma tumors, especially in cases with high levels of tumor-infiltrating lymphocytes (TILs). The response rate is typically higher in patients with melanoma compared to other tumor types.
- Lung Cancer: Immunotherapy, often in combination with chemotherapy, has demonstrated promising results in non-small cell lung cancer. The combination therapy strategy aims to leverage the strengths of both approaches to maximize anti-tumor effects.
- Renal Cell Carcinoma: Immune checkpoint inhibitors have shown effectiveness in treating renal cell carcinoma, particularly in patients with advanced or metastatic disease.
Final Review
In conclusion, immunotherapy’s ability to shrink tumors without surgery presents a significant advancement in cancer care. While challenges remain, including potential side effects and the need for personalized treatment approaches, the early results are extremely promising. Future research and development in immunotherapy hold the potential to transform cancer treatment, offering more effective and less invasive options for patients.




