Hyperkalemia causes risk factors sets the stage for understanding this potentially serious health condition. High potassium levels, or hyperkalemia, can arise from various sources, including underlying medical issues, medications, and lifestyle choices. Understanding these causes and associated risk factors is crucial for early detection and effective management. This comprehensive guide will delve into the mechanisms behind hyperkalemia, examining the diverse range of factors that contribute to its development.
This in-depth exploration will cover the various causes, from kidney dysfunction to cellular breakdown, and will examine the risk factors that make some individuals more susceptible to hyperkalemia. We will also discuss the critical role of preventative measures and how to manage this condition effectively.
Introduction to Hyperkalemia
Hyperkalemia is a potentially life-threatening condition characterized by an abnormally high level of potassium in the blood. Understanding its mechanisms, causes, and severity is crucial for timely diagnosis and appropriate treatment. Maintaining a balanced potassium level is essential for the proper functioning of various organs, including the heart, muscles, and nerves.Potassium, a vital electrolyte, plays a critical role in numerous bodily functions.
Hyperkalemia, a condition where potassium levels get too high, can have various causes, including kidney problems and certain medications. Understanding these risk factors is crucial for preventative measures. Interestingly, similar to managing dry age-related macular degeneration (AMD), which is often treated with lifestyle changes and potentially supplements, careful dietary management plays a role in preventing hyperkalemia. Learning more about how dry AMD is treated can offer insights into the importance of proactive health strategies.
For a deeper dive into dry AMD treatment options, check out this informative resource: how dry amd is treated. Ultimately, addressing the causes and risk factors for hyperkalemia is key to maintaining good health.
Normal potassium levels are tightly regulated within a specific range, and deviations from this range can lead to significant health consequences. The body employs intricate mechanisms to maintain potassium homeostasis, preventing excessive accumulation or depletion. These mechanisms include renal excretion, dietary intake, and intracellular shifts.
Normal Potassium Levels and Homeostasis
Potassium levels in the blood are typically maintained within a narrow range. The normal serum potassium level is generally considered to be between 3.5 and 5.0 milliequivalents per liter (mEq/L). Deviations from this range can lead to various physiological disturbances. The body employs several mechanisms to regulate potassium levels, ensuring its concentration remains stable. These include:
- Renal Excretion: The kidneys play a crucial role in eliminating excess potassium from the body through urine. Changes in dietary intake, kidney function, and hormonal influences directly affect potassium excretion.
- Dietary Intake: Potassium is obtained through various dietary sources. A balanced diet that includes fruits, vegetables, and other potassium-rich foods is important for maintaining optimal potassium levels. Conversely, excessive intake or the use of certain medications can lead to imbalances.
- Intracellular Shifts: Potassium moves between the intracellular and extracellular fluid compartments in response to various factors. Changes in pH, insulin activity, and cellular processes can influence the distribution of potassium, impacting its serum levels.
Categories of Hyperkalemia
Classifying hyperkalemia helps determine the appropriate treatment approach and potential severity. Different categories consider factors like the rate of onset and the degree of elevation.
| Category | Description | Severity | Examples |
|---|---|---|---|
| Acute Hyperkalemia | Characterized by a rapid increase in serum potassium levels. | Potentially life-threatening due to rapid onset. | Severe dehydration, kidney failure, medications that impair potassium excretion |
| Chronic Hyperkalemia | Involves a gradual increase in serum potassium levels over time. | May be less acutely dangerous but can still cause significant harm if left untreated. | Chronic kidney disease, adrenal insufficiency, certain medications |
| Mild Hyperkalemia | Serum potassium levels slightly above the normal range (e.g., 5.1-6.0 mEq/L). | Usually manageable with appropriate interventions. | Sometimes a symptom of underlying conditions, or a side effect of certain medications |
| Severe Hyperkalemia | Serum potassium levels significantly elevated (e.g., greater than 7.0 mEq/L). | Potentially fatal, requiring immediate medical intervention. | Acute kidney injury, severe acidosis |
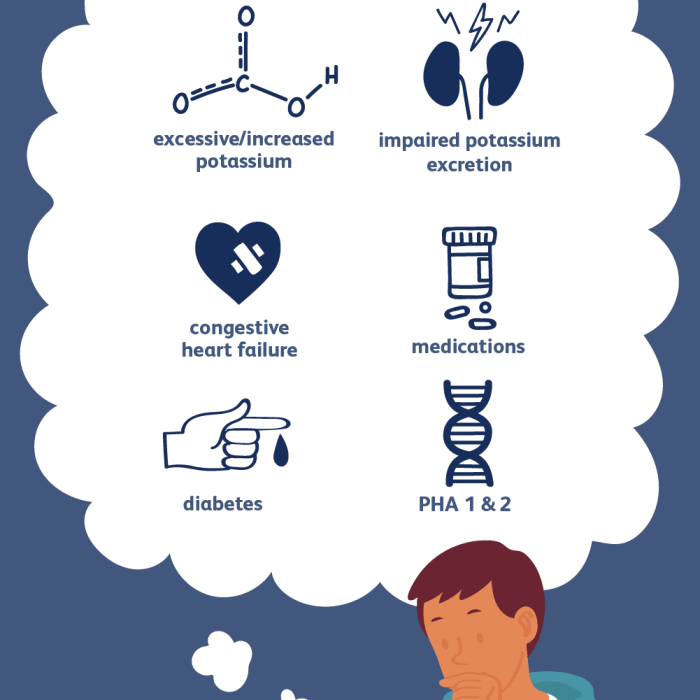
Causes of Hyperkalemia: Hyperkalemia Causes Risk Factors
Hyperkalemia, a condition characterized by excessively high levels of potassium in the blood, can have various underlying causes. Understanding these causes is crucial for prompt diagnosis and effective treatment. Early identification and intervention can significantly reduce the risk of serious complications.Potassium, a vital electrolyte, plays a critical role in numerous bodily functions, including nerve impulse transmission and muscle contraction.
Disruptions in the balance of potassium, either through intake or excretion, can lead to hyperkalemia. This imbalance can stem from a multitude of medical conditions, medications, and lifestyle factors.
Medical Conditions Associated with Hyperkalemia
Several medical conditions can impair the body’s ability to eliminate potassium, leading to elevated blood levels. These conditions often involve kidney dysfunction, affecting the kidneys’ crucial role in filtering waste products, including excess potassium.
- Kidney Disease: Chronic kidney disease (CKD) and acute kidney injury (AKI) are prominent causes. Damaged kidneys struggle to effectively filter potassium from the blood, resulting in its accumulation. For example, a patient with advanced CKD may experience progressive hyperkalemia requiring dialysis to remove excess potassium.
- Addison’s Disease: This adrenal insufficiency disorder affects the body’s ability to regulate hormones, including aldosterone, which is vital for potassium excretion. The reduced aldosterone production can lead to a buildup of potassium in the blood.
- Dehydration: Severe dehydration can lead to hyperkalemia. When fluid intake is insufficient, the concentration of potassium in the blood increases, as the body’s fluid volume decreases.
- Acidosis: Metabolic acidosis, characterized by a decrease in blood pH, can shift potassium from cells into the bloodstream. This shift contributes to elevated potassium levels. For instance, diabetic ketoacidosis can result in significant acidosis and hyperkalemia.
- Hypoaldosteronism: A condition where the adrenal glands don’t produce enough aldosterone. Aldosterone is crucial for regulating sodium and potassium balance, and its deficiency disrupts this balance, leading to hyperkalemia.
Medications Leading to Hyperkalemia
Certain medications can interfere with potassium excretion or increase potassium intake, potentially leading to hyperkalemia. Patients taking these medications should be monitored for signs of elevated potassium levels.
- Potassium-Sparing Diuretics: These medications help retain potassium, thereby increasing blood levels. Examples include spironolactone and amiloride.
- ACE Inhibitors and ARBs: Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) are frequently prescribed for hypertension. However, they can also lead to hyperkalemia in susceptible individuals.
- NSAIDs: Nonsteroidal anti-inflammatory drugs (NSAIDs) can impair kidney function, potentially contributing to hyperkalemia, especially in patients with pre-existing kidney disease.
- Heparin: In some cases, heparin use can lead to hyperkalemia, especially in combination with other medications.
- Cyclosporine: This immunosuppressant medication can affect kidney function, increasing the risk of hyperkalemia.
Kidney Dysfunction in Hyperkalemia
Kidney dysfunction plays a central role in hyperkalemia. The kidneys’ primary function in potassium homeostasis is to filter and excrete excess potassium from the body. Compromised kidney function leads to reduced potassium excretion, resulting in elevated blood levels.
Cellular Breakdown and Hyperkalemia
Cellular breakdown, such as that seen in severe muscle trauma or burns, releases intracellular potassium into the bloodstream. This rapid release can overwhelm the kidneys’ ability to excrete the potassium, resulting in hyperkalemia.
Comparison of Hyperkalemia Causes
| Cause | Mechanism | Risk Factors | Examples |
|---|---|---|---|
| Kidney Disease | Impaired potassium excretion | Diabetes, high blood pressure, family history | Chronic kidney disease, acute kidney injury |
| Medications | Increased potassium retention or reduced excretion | Pre-existing kidney conditions, concurrent medications | Potassium-sparing diuretics, ACE inhibitors |
| Cellular Breakdown | Release of intracellular potassium | Crush injuries, burns, rhabdomyolysis | Severe muscle trauma, extensive burns |
| Addison’s Disease | Reduced aldosterone production | Autoimmune disorders | Adrenal insufficiency |
Risk Factors for Hyperkalemia
Hyperkalemia, a condition characterized by dangerously high levels of potassium in the blood, can have severe consequences if left untreated. Understanding the risk factors associated with this condition is crucial for prevention and early intervention. Identifying individuals at higher risk allows for targeted interventions and monitoring, potentially preventing life-threatening complications.
High potassium levels, or hyperkalemia, can stem from various factors like kidney problems or certain medications. Understanding the causes and risk factors is crucial for preventative care. Interestingly, some similar symptoms can arise with mononucleosis (mono), which can be tricky to diagnose. To learn more about how doctors diagnose mono, check out this helpful guide: how is mono diagnosed.
Ultimately, pinpointing the causes of hyperkalemia involves a thorough evaluation by a healthcare professional.
Demographic Factors
Several demographic factors influence the likelihood of developing hyperkalemia. Age and sex, for example, play a significant role in susceptibility. Age-related changes in kidney function can impact potassium regulation, making older adults more vulnerable. Additionally, certain underlying health conditions can disproportionately affect individuals of particular genders, increasing their risk.
- Age: Kidney function often declines with age, impacting the body’s ability to efficiently filter potassium from the blood. This makes older adults, particularly those over 65, more susceptible to hyperkalemia.
- Sex: While research shows no significant difference in the prevalence of hyperkalemia between genders, certain underlying conditions more commonly affecting one sex may contribute to an increased risk. For example, individuals with kidney disease, which is more prevalent in certain age groups, may experience hyperkalemia.
Nutritional Factors
Dietary choices significantly impact potassium levels. A diet high in potassium-rich foods, combined with impaired kidney function, can lead to hyperkalemia. Excessive potassium intake, especially in individuals with kidney disease, poses a considerable risk.
- High Potassium Intake: Individuals consuming substantial amounts of potassium-rich foods, such as bananas, oranges, spinach, and potatoes, may be at higher risk if their kidneys cannot effectively excrete the excess potassium. This is particularly relevant for those with pre-existing kidney issues.
- Supplements: Potassium supplements are frequently used to address low potassium levels, but they can easily lead to hyperkalemia if not carefully monitored, especially in individuals with kidney problems.
Lifestyle Factors
Certain lifestyle choices can increase the risk of hyperkalemia. Medications and specific dietary patterns can have a profound effect. Lack of physical activity or specific medical conditions can also contribute.
- Medications: Many medications, including some diuretics, ACE inhibitors, and NSAIDs, can negatively impact kidney function, increasing the risk of hyperkalemia. Patients taking multiple medications should closely monitor their potassium levels, particularly if they have underlying kidney conditions.
- Limited Physical Activity: A sedentary lifestyle may impact the body’s ability to regulate potassium levels, contributing to an increased risk of hyperkalemia.
Patient Populations at Higher Risk
Certain patient populations are inherently more vulnerable to hyperkalemia due to underlying health conditions. Individuals with chronic kidney disease (CKD), diabetes, and those undergoing certain medical procedures, such as dialysis, are at higher risk. Early detection and proactive management are crucial for these groups.
- Chronic Kidney Disease (CKD): Individuals with CKD often experience impaired kidney function, making them more prone to hyperkalemia. Their kidneys struggle to remove excess potassium from the blood, leading to potentially dangerous levels.
- Diabetic Patients: Diabetic nephropathy (kidney damage associated with diabetes) can increase the risk of hyperkalemia. The impact of diabetes on kidney function and the associated medications can create a higher susceptibility to potassium imbalances.
Categorization of Risk Factors
| Category | Type | Description | Examples |
|---|---|---|---|
| Modifiable | Lifestyle | Factors that can be changed or controlled. | Diet, exercise, medication use |
| Modifiable | Medical | Factors that can be addressed through medical interventions. | Underlying conditions like kidney disease, diabetes |
| Non-Modifiable | Demographic | Factors that cannot be changed. | Age, sex |
Clinical Manifestations of Hyperkalemia
Hyperkalemia, a condition characterized by elevated potassium levels in the blood, can manifest in a range of symptoms, from mild discomfort to life-threatening complications. Understanding these manifestations is crucial for prompt diagnosis and effective treatment. Early recognition and intervention are vital to prevent severe consequences.
Symptoms of Hyperkalemia, Hyperkalemia causes risk factors
The symptoms of hyperkalemia often emerge gradually, progressing from mild to severe as the potassium level rises. Initial symptoms might be subtle and easily overlooked, making early detection challenging. Symptoms can include general malaise, nausea, and vomiting. As the condition worsens, more significant symptoms appear, and it is crucial to be aware of the potential escalation.
Physical Signs of Hyperkalemia
Physical examination plays a vital role in assessing the severity of hyperkalemia. Early physical signs might include muscle weakness or cramping, which can progress to more severe muscle paralysis if the condition is not managed promptly. Other physical findings might include paresthesias (tingling or numbness) in the extremities. The severity of these physical signs often correlates with the potassium level.
Electrocardiographic (ECG) Changes Associated with Hyperkalemia
Electrocardiography (ECG) is a critical tool in evaluating hyperkalemia. Specific ECG changes are associated with different stages of hyperkalemia. Early changes might be subtle, but as the potassium level rises, more pronounced and potentially life-threatening changes appear. These changes often manifest as characteristic patterns that indicate the need for immediate intervention. These changes are often observed in the form of progressively increasing peaked T waves, widening QRS complexes, and ultimately, a sine wave pattern, which is a serious and ominous sign.
Understanding the ECG changes is crucial for prompt diagnosis and treatment.
Variation in Symptoms Based on Severity and Duration
The symptoms of hyperkalemia can vary significantly based on the severity and duration of the elevated potassium level. Mild elevations might cause only subtle symptoms, while severe and prolonged hyperkalemia can lead to serious and even life-threatening complications. This variability emphasizes the importance of monitoring potassium levels and recognizing early signs, even if they are subtle. For example, a gradual increase in potassium over a longer period might present with more subtle symptoms, such as fatigue and muscle weakness, compared to a rapid increase in potassium, which may cause more pronounced symptoms like severe muscle weakness and cardiac arrhythmias.
Table of Symptoms, Physical Signs, and ECG Changes in Hyperkalemia
| Symptom | Physical Sign | ECG Change | Severity |
|---|---|---|---|
| Muscle weakness/cramps | Decreased muscle tone, difficulty with movement | Peaked T waves | Mild |
| Paresthesias (tingling/numbness) | Numbness or tingling in extremities | Widened QRS complex | Moderate |
| Nausea/vomiting | Unexplained feelings of nausea, followed by vomiting | Prolonged PR interval | Moderate |
| Abdominal cramping | Severe cramping in the abdomen | Loss of P waves | Severe |
| Cardiac arrest | Loss of cardiac function | Sine wave pattern | Life-threatening |
Diagnosis of Hyperkalemia
Hyperkalemia, a potentially life-threatening condition characterized by elevated potassium levels in the blood, necessitates prompt and accurate diagnosis. Early detection allows for immediate intervention and minimizes the risk of severe complications. This crucial step involves a combination of laboratory tests and electrocardiogram (ECG) analysis, which will be explored in detail below.
Diagnostic Tests for Hyperkalemia
Identifying hyperkalemia requires a systematic approach. Initial suspicion is often triggered by a patient’s medical history, symptoms, and physical examination. Crucial diagnostic tools include serum potassium levels, kidney function tests, and electrocardiogram (ECG) analysis. These tests provide critical insights into the severity and underlying cause of the elevated potassium.
Interpretation of Serum Potassium Levels
Serum potassium levels are a cornerstone of hyperkalemia diagnosis. The normal range for serum potassium typically falls between 3.5 and 5.0 milliequivalents per liter (mEq/L). Levels exceeding this range indicate hyperkalemia. A critical aspect of interpretation is recognizing that the clinical significance of a particular potassium level is context-dependent and requires careful consideration of other factors, including the patient’s overall health, underlying conditions, and medication use.
For example, a patient with chronic kidney disease may have a slightly elevated potassium level without experiencing significant symptoms, whereas a healthy individual with a similar potassium level might exhibit severe symptoms.
Monitoring Kidney Function Tests in Hyperkalemia Diagnosis
Kidney function tests are essential in evaluating the cause and severity of hyperkalemia. Since the kidneys play a critical role in potassium excretion, any impairment in renal function can lead to potassium buildup in the bloodstream. Assessing creatinine levels, blood urea nitrogen (BUN), and glomerular filtration rate (GFR) is crucial to determine the degree of kidney dysfunction and its contribution to the hyperkalemia.
For instance, patients with chronic kidney disease (CKD) often have impaired kidney function, which directly impacts their ability to filter potassium. This impairment necessitates careful monitoring and management of potassium levels.
Role of ECG in the Diagnostic Process
Electrocardiogram (ECG) analysis is a vital tool for assessing the cardiac effects of hyperkalemia. Changes in ECG patterns can be indicative of increasing potassium levels and subsequent cardiac complications. Early identification of these ECG changes allows for prompt treatment and mitigation of potential life-threatening arrhythmias. ECG abnormalities associated with hyperkalemia may include peaked T waves, shortened QT intervals, and eventually, complete heart block, each representing increasing severity.
Diagnostic Procedures for Hyperkalemia
| Diagnostic Procedure | Expected Results (Hyperkalemia) | Interpretation | Clinical Significance |
|---|---|---|---|
| Serum Potassium Level | > 5.0 mEq/L | Elevated potassium level | Indicates hyperkalemia; further investigation needed. |
| Kidney Function Tests (Creatinine, BUN, GFR) | Abnormal values (e.g., elevated creatinine, reduced GFR) | Indicates kidney dysfunction. | Suggests a potential contributing factor to hyperkalemia. |
| ECG | Peaked T waves, shortened QT intervals, widened QRS complexes, or complete heart block | ECG changes indicative of hyperkalemia | Indicates potential cardiac compromise; immediate intervention is required. |
Management of Hyperkalemia
Hyperkalemia, a condition characterized by dangerously high levels of potassium in the blood, requires prompt and effective management to prevent severe complications and even death. Early intervention is crucial to stabilize the patient’s condition and mitigate the risk of cardiac arrhythmias. Different treatment strategies are employed depending on the severity of hyperkalemia, ranging from simple lifestyle modifications to more intensive interventions like dialysis.
Treatment Options for Hyperkalemia
Treatment for hyperkalemia focuses on rapidly lowering serum potassium levels and addressing the underlying cause. This involves a multifaceted approach, utilizing a combination of medications, intravenous fluids, and, in severe cases, dialysis. The goal is to prevent the potentially fatal effects of hyperkalemia on the heart.
High potassium levels, or hyperkalemia, can stem from various factors, including kidney problems and certain medications. Interestingly, a rheumatoid arthritis flare up can sometimes lead to electrolyte imbalances, which could contribute to hyperkalemia. Understanding these potential connections is crucial for effective management of hyperkalemia causes and risk factors.
Role of Intravenous Fluids
Intravenous (IV) fluids play a significant role in managing hyperkalemia. They help to dilute the potassium concentration in the blood, thereby reducing the risk of cardiac complications. Rapid infusion of isotonic saline solutions, such as 0.9% sodium chloride, is often the first-line treatment for acute hyperkalemia. This action facilitates the shift of potassium from the extracellular to the intracellular compartment.
The effectiveness of this strategy is directly related to the rate of fluid administration and the patient’s overall condition. Administering fluids, however, should not be done alone, and should be accompanied by other treatment options, as discussed below.
Role of Medications
Several medications are employed to manage hyperkalemia, either to reduce potassium absorption or to promote its excretion. These medications work through different mechanisms. For example, calcium gluconate is frequently used to stabilize cardiac membranes, countering the effects of hyperkalemia on the heart. Insulin, combined with glucose, promotes potassium uptake into cells. Furosemide and other loop diuretics enhance potassium excretion through the kidneys.
The selection of medication and the dosage will depend on the severity of the condition and the patient’s overall health status.
Use of Dialysis in Severe Hyperkalemia
In severe cases of hyperkalemia, where other treatments are insufficient or contraindicated, dialysis becomes a crucial intervention. Dialysis effectively removes excess potassium from the blood. Hemodialysis and peritoneal dialysis are the most common types used in such situations. The efficacy of dialysis is directly related to the speed and duration of the treatment session. In patients with chronic kidney disease, dialysis is often a crucial component of long-term management.
Steps in Managing an Acute Hyperkalemia Crisis
Managing an acute hyperkalemia crisis involves a rapid sequence of interventions to stabilize the patient’s condition. A thorough assessment of the patient’s vital signs, including heart rate and rhythm, is paramount. Intravenous access should be established immediately. The initial treatment steps usually involve administering IV calcium gluconate to stabilize the heart, followed by insulin and glucose to promote potassium uptake into cells.
If these measures prove insufficient, dialysis may be necessary.
Treatment Approach Based on Severity
The severity of hyperkalemia directly influences the treatment approach. Mild hyperkalemia might only require monitoring and lifestyle modifications. Moderate hyperkalemia typically involves intravenous fluids and medications to lower potassium levels. Severe hyperkalemia, on the other hand, often requires prompt dialysis to quickly remove the excess potassium and stabilize the patient’s condition. The severity is determined by the serum potassium levels and the patient’s clinical presentation.
Comparison of Treatment Approaches
| Treatment Approach | Advantages | Disadvantages | Considerations |
|---|---|---|---|
| Intravenous Fluids | Rapidly lowers serum potassium, relatively safe | May not be sufficient for severe cases, potential for fluid overload | Assess for fluid intolerance, monitor for adverse effects |
| Medications (e.g., Calcium Gluconate, Insulin, Diuretics) | Effective in lowering potassium, can be administered quickly | May have side effects, may not be effective alone in severe cases, need careful monitoring | Monitor for adverse effects, adjust dosage based on patient response |
| Dialysis | Highly effective in removing excess potassium, life-saving in severe cases | Requires specialized equipment and trained personnel, may have potential complications | Assess for need based on severity, consider patient’s overall health status |
Prognosis and Prevention
Hyperkalemia, if left untreated, can lead to serious complications and potentially life-threatening outcomes. Understanding the potential risks and preventative measures is crucial for managing this condition effectively. Proactive strategies for identifying and addressing modifiable risk factors play a key role in preventing future episodes and improving long-term health.Untreated hyperkalemia can progress to severe complications, affecting various organ systems and potentially leading to cardiac arrest.
The severity of these complications often depends on the degree and duration of elevated potassium levels, as well as the presence of underlying health conditions. Proactive measures to mitigate the risk of hyperkalemia are therefore vital. Implementing these measures can help prevent serious health issues.
Potential Complications of Untreated Hyperkalemia
Untreated hyperkalemia can result in a cascade of serious complications, primarily affecting the cardiovascular system. Symptoms can range from mild muscle weakness to life-threatening cardiac arrhythmias. Early detection and intervention are essential to prevent these complications from escalating.Cardiac arrhythmias are a primary concern. Elevated potassium levels can disrupt the electrical activity of the heart, potentially leading to dangerous heart rhythms like ventricular fibrillation or asystole.
These arrhythmias can rapidly progress to cardiac arrest, necessitating immediate medical intervention. Other severe complications include neuromuscular issues, characterized by muscle weakness, paralysis, and even respiratory failure. In severe cases, the buildup of potassium can directly affect the kidneys, potentially leading to acute kidney injury or chronic kidney disease.
Preventative Strategies to Reduce Hyperkalemia Risk
Implementing preventative strategies is crucial in reducing the risk of hyperkalemia. These strategies focus on identifying and addressing modifiable risk factors and promoting lifestyle changes. The goal is to maintain healthy potassium levels and reduce the likelihood of future episodes.Effective preventative strategies include careful medication management, particularly for patients on medications that can elevate potassium levels. Monitoring dietary potassium intake is also essential.
A balanced diet with appropriate potassium intake is vital. For example, patients with kidney disease require specific dietary adjustments to manage potassium levels effectively. Regular blood tests to monitor potassium levels are important to ensure early detection of any potential imbalances.
Strategies to Identify and Address Modifiable Risk Factors
Identifying and addressing modifiable risk factors is key to preventing hyperkalemia. These factors often stem from underlying medical conditions, medication use, and lifestyle choices. Proactive management of these factors can significantly reduce the risk of hyperkalemia.Careful medication review is crucial. Medications that can contribute to elevated potassium levels should be identified and potentially adjusted. For example, certain potassium-sparing diuretics or medications used to treat conditions like hypertension or heart failure need to be carefully monitored.
Furthermore, addressing underlying health conditions like kidney disease, diabetes, or adrenal insufficiency is critical in managing potential potassium imbalances. Patient education on potassium-rich foods is essential, and strategies for managing potassium intake should be implemented.
Table of Potential Complications, Preventative Strategies, and Outcomes
| Potential Complications | Preventative Strategies | Associated Outcomes | Example Scenarios |
|---|---|---|---|
| Cardiac Arrhythmias (e.g., ventricular fibrillation) | Medication review, regular potassium monitoring, dietary adjustments | Reduced risk of cardiac arrest, improved cardiac function | A patient with a history of heart failure and taking ACE inhibitors, whose potassium levels are monitored and adjusted, may prevent life-threatening arrhythmias. |
| Neuromuscular Issues (e.g., muscle weakness, paralysis) | Dietary modifications, appropriate medication adjustments | Improved muscle function, reduced risk of respiratory failure | A patient with kidney disease following a dietary plan to limit potassium intake will likely experience less muscle weakness and fewer respiratory issues. |
| Acute Kidney Injury/Chronic Kidney Disease | Regular kidney function monitoring, careful management of underlying conditions | Preservation of kidney function, reduced risk of kidney failure | Patients with pre-existing kidney disease who maintain a strict potassium-controlled diet and monitor kidney function frequently are likely to avoid complications. |
| Severe Metabolic Acidosis | Monitoring and managing underlying conditions, prompt treatment of hyperkalemia | Reduced risk of organ damage, improved overall metabolic health | Prompt intervention in patients with diabetes or other conditions prone to metabolic acidosis can prevent severe organ damage from hyperkalemia. |
Ending Remarks
In conclusion, hyperkalemia, characterized by elevated potassium levels, presents a complex interplay of causes and risk factors. Understanding the diverse mechanisms behind its development, from underlying medical conditions to lifestyle choices, is paramount for proactive health management. By recognizing the modifiable and non-modifiable risk factors, individuals can take steps to mitigate their risk and ensure prompt intervention should hyperkalemia occur.
Early detection and effective management are crucial to prevent potential complications and maintain overall well-being.




