Multiple sclerosis diagnostic criteria are crucial for accurate and timely diagnosis. Understanding these criteria is vital for healthcare professionals and individuals affected by MS. This guide delves into the historical evolution, clinical manifestations, diagnostic tests, imaging techniques, neurological examinations, and diagnostic guidelines. It provides a comprehensive overview of the process from initial symptoms to definitive diagnosis.
This detailed exploration of multiple sclerosis diagnostic criteria will provide a structured understanding of the various steps involved in identifying and confirming the condition. The key characteristics of a comprehensive diagnostic approach will be highlighted, along with specific examples of symptoms, tests, and criteria used in clinical practice.
Introduction to Multiple Sclerosis Diagnostic Criteria
Multiple sclerosis (MS) is a chronic, autoimmune disease affecting the central nervous system. It’s characterized by inflammation and demyelination, disrupting the communication pathways between the brain, spinal cord, and the rest of the body. Symptoms can vary significantly, making accurate diagnosis challenging.Accurate diagnostic criteria are crucial for timely and appropriate management of MS. Misdiagnosis can lead to delayed treatment, impacting the progression of the disease and quality of life.
Clear diagnostic guidelines ensure consistency in diagnosis across different healthcare settings and facilitate research into MS.
Historical Evolution of MS Diagnostic Criteria
The understanding and diagnosis of MS have evolved significantly over time. Early diagnostic approaches relied on clinical observations and symptoms, leading to inconsistent diagnoses. The development of more sophisticated diagnostic tools, including neuroimaging techniques, has refined the process, leading to more accurate identification of MS. The shift from primarily clinical criteria to a combination of clinical and paraclinical findings has improved diagnostic accuracy.
Early criteria emphasized the clinical presentation of disseminated lesions in space and time. Modern criteria incorporate neurological examination, magnetic resonance imaging (MRI) findings, and evoked potential studies. This evolution demonstrates a continuous refinement in diagnostic strategies, reflecting the increasing understanding of the disease.
Key Characteristics of a Comprehensive Diagnostic Approach to MS
A comprehensive approach to MS diagnosis requires a multifaceted assessment encompassing clinical evaluation, neuroimaging, and ancillary tests. The primary goal is to confirm the diagnosis of MS while ruling out other conditions with similar symptoms. This necessitates careful consideration of the patient’s medical history, neurological examination findings, and laboratory results. It also includes a comprehensive evaluation of the patient’s clinical picture to establish the diagnosis of MS.
It necessitates meticulous consideration of the patient’s medical history, neurological examination findings, and laboratory results.
Diagnostic Process Summary
The following table summarizes the key components of the MS diagnostic process. Accurate diagnosis hinges on a thorough evaluation, ensuring that the symptoms align with the established criteria for MS and that other potential causes are excluded.
| Component | Description | Examples |
|---|---|---|
| Medical History | Detailed review of the patient’s symptoms, including their onset, progression, and characteristics. Past medical history, including any relevant autoimmune disorders, is also important. | Symptom duration, frequency, and location; any prior neurological events; medication history; family history of neurological disorders. |
| Neurological Examination | Comprehensive assessment of the patient’s neurological function, including motor skills, sensory perception, coordination, balance, and reflexes. This helps identify specific neurological deficits. | Muscle strength, sensation, reflexes, coordination, balance, cranial nerve function. |
| Neuroimaging (MRI) | Magnetic resonance imaging (MRI) scans are crucial for identifying lesions in the brain and spinal cord. These lesions are crucial indicators of demyelination. | Presence of demyelinating lesions in different regions of the brain and spinal cord. The distribution and characteristics of lesions help distinguish MS from other conditions. |
| Ancillary Tests | Additional tests like evoked potential studies and cerebrospinal fluid (CSF) analysis may be used to further evaluate the neurological status. | Visual evoked potentials (VEPs), auditory brainstem responses (ABRs), and CSF analysis for oligoclonal bands, indicative of immune system involvement. |
Clinical Manifestations and Symptoms
Multiple sclerosis (MS) is a chronic, autoimmune disease affecting the central nervous system. The hallmark of MS is the unpredictable nature of its presentation, with symptoms varying greatly in type, severity, and frequency depending on the individual and the specific areas of the brain and spinal cord affected. Understanding the spectrum of neurological symptoms is crucial for early diagnosis and effective management.The symptoms of MS are often subtle and can mimic other neurological conditions.
Figuring out multiple sclerosis diagnostic criteria can be tricky, often involving a combination of factors. While some symptoms might be subtle, like vision changes, it’s important to remember that excess fluid in the eyes, for example, can have various causes, treatments, and types. This can sometimes be misconstrued as an early sign, and it’s important to remember that multiple sclerosis diagnostic criteria require a comprehensive approach and often involve ruling out other conditions.
Further research into excess fluid in eyes types causes treatment can help understand related eye symptoms. Ultimately, the diagnostic process for multiple sclerosis relies on a thorough medical evaluation.
Early detection relies heavily on recognizing patterns in symptom presentation, duration, and frequency. Identifying common initial symptoms and understanding the diverse ways MS manifests are critical for prompt medical intervention.
Spectrum of Neurological Symptoms
MS symptoms stem from demyelination, the breakdown of the protective myelin sheath surrounding nerve fibers. This disruption interferes with nerve signal transmission, leading to a wide range of neurological deficits. These can range from mild, intermittent symptoms to debilitating, progressive impairments. Common symptoms include visual disturbances, motor weakness, sensory changes, and cognitive difficulties.
Common Initial Symptoms
Initial symptoms of MS can be diverse, and often subtle. Common initial complaints include: optic neuritis (inflammation of the optic nerve), characterized by pain and vision loss; numbness or tingling in limbs, often starting in one extremity; weakness in one or more limbs, causing difficulty with walking or fine motor skills; dizziness and balance problems, potentially leading to falls.
Recognizing the early indicators is critical for early diagnosis and appropriate treatment.
Symptom Duration and Pattern
The duration and pattern of symptoms are vital diagnostic clues. Symptoms of MS are often characterized by periods of exacerbations (worsening of symptoms) followed by periods of remission (improvement or stabilization). The unpredictable nature of symptom onset and progression, as well as the fluctuating patterns, make diagnosis challenging. The duration and frequency of these attacks are significant indicators for the disease.
Neurological Deficits
MS can manifest in various neurological deficits, impacting different aspects of functioning. Visual disturbances, such as blurry vision, double vision, or loss of vision, are common. Motor deficits, ranging from mild weakness in one limb to significant paralysis, can affect movement and coordination. Sensory changes, including numbness, tingling, or pain, are frequently reported. Cognitive impairments, such as problems with memory, concentration, or executive functions, can also be present.
Evaluation and Documentation of Symptoms
Thorough evaluation and meticulous documentation of symptoms are crucial for diagnosis. Neurological examinations, including assessments of motor function, sensory perception, reflexes, coordination, and cranial nerve function, are essential components. Detailed patient histories, including symptom onset, duration, frequency, and any associated factors, are vital. Symptom diaries, where patients record their symptoms, severity, and triggers, are invaluable tools.
Table of Common Symptoms and Severity
| Symptom | Potential Severity |
|---|---|
| Visual disturbances (e.g., blurry vision, double vision, optic neuritis) | Mild to severe, potentially leading to significant vision loss |
| Motor weakness (e.g., limb weakness, ataxia) | Mild to severe, potentially impacting mobility and daily activities |
| Sensory changes (e.g., numbness, tingling, pain) | Mild to severe, affecting sensation and potentially causing discomfort |
| Cognitive impairments (e.g., memory problems, concentration difficulties) | Mild to severe, affecting daily life activities |
| Balance and coordination problems (e.g., dizziness, falls) | Mild to severe, potentially leading to falls and injuries |
| Fatigue | Variable, from mild tiredness to debilitating exhaustion, impacting daily activities. |
Diagnostic Tests and Procedures: Multiple Sclerosis Diagnostic Criteria
Unveiling the intricate world of multiple sclerosis (MS) diagnosis often involves a multifaceted approach, relying on a combination of clinical evaluations and various diagnostic tests. This process aims to confirm the presence of MS, identify its characteristics, and distinguish it from other neurological conditions with similar symptoms. Accurate diagnosis is crucial for timely and effective treatment planning.Neurological examinations, while crucial, often provide suggestive evidence rather than definitive proof of MS.
Consequently, supplementary tests play a pivotal role in the diagnostic journey. These tests are designed to identify characteristic patterns in the central nervous system (CNS) that suggest the presence of MS, helping to differentiate it from other conditions with overlapping symptoms. The combination of clinical findings and test results allows healthcare professionals to arrive at a precise diagnosis.
Magnetic Resonance Imaging (MRI)
MRI scans are paramount in MS diagnosis, providing detailed images of the brain and spinal cord. The procedure involves placing the patient inside a large, magnetic machine. Radio waves and a strong magnetic field are used to create detailed cross-sectional images. Specific MRI protocols, such as gadolinium-enhanced scans, are employed to identify areas of inflammation, a hallmark of MS lesions.
Interpreting MRI results requires specialized knowledge, as subtle changes can be indicative of MS. A pattern of demyelination, or the loss of the protective myelin sheath around nerve fibers, is a significant indicator. The location, size, and number of lesions observed are crucial factors in evaluating the likelihood of MS. However, MRI findings alone may not be conclusive, and must be considered in conjunction with clinical presentation and other tests.
Evoked Potentials
Evoked potentials assess the speed of nerve impulses traveling along specific pathways in the nervous system. These tests measure the time it takes for electrical signals to travel from a stimulus to the brain. Different types of evoked potentials exist, each targeting specific pathways. For example, visual evoked potentials (VEPs) evaluate visual pathways, while auditory brainstem responses (ABRs) assess auditory pathways.
The procedure involves applying stimuli (e.g., visual flashes, sounds) and recording the brain’s electrical response. The interpretation focuses on the latency (delay) and amplitude (strength) of the responses. Variations in these parameters can indicate abnormalities in nerve conduction, potentially suggestive of MS. However, the absence of abnormal results does not definitively rule out MS, as other conditions can also affect nerve conduction.
Cerebrospinal Fluid (CSF) Analysis
CSF analysis involves obtaining a sample of cerebrospinal fluid, the fluid surrounding the brain and spinal cord. The procedure involves a lumbar puncture, a minimally invasive procedure where a needle is inserted into the lower back to collect the CSF. The collected CSF is then analyzed for specific proteins, antibodies, and immune cells. Elevated levels of specific proteins, such as oligoclonal bands (OCBs), can be indicative of MS.
These bands are proteins produced by the immune system and are often present in higher concentrations in the CSF of individuals with MS. The interpretation of CSF results requires careful consideration of the presence and quantity of OCBs in conjunction with other diagnostic findings. The presence of OCBs, while supportive of an MS diagnosis, isn’t always definitive.
Table of Diagnostic Tests
| Test | Procedure | Interpretation | Limitations |
|---|---|---|---|
| MRI | Patient placed inside a large magnetic machine; radio waves and magnetic field create detailed images. | Presence of demyelinating lesions in the brain and spinal cord. | MRI findings alone may not be conclusive; other conditions may exhibit similar patterns. |
| Evoked Potentials | Stimuli (e.g., visual flashes, sounds) are applied, and the brain’s electrical response is recorded. | Abnormal latency or amplitude of responses may suggest nerve conduction issues. | Absence of abnormalities doesn’t definitively rule out MS; other conditions can affect nerve conduction. |
| CSF Analysis | Lumbar puncture to collect cerebrospinal fluid; the fluid is then analyzed for proteins, antibodies, and immune cells. | Elevated levels of specific proteins (e.g., oligoclonal bands) can be indicative of MS. | Presence of OCBs isn’t always definitive; other conditions may have similar findings. |
Imaging Techniques
Magnetic Resonance Imaging (MRI) has become the cornerstone of multiple sclerosis (MS) diagnosis. It provides crucial visual information about the central nervous system, allowing neurologists to identify characteristic lesions that are indicative of MS. This detailed visualization is critical in distinguishing MS from other neurological conditions with similar symptoms.MRI’s non-invasive nature and exceptional soft tissue contrast make it an invaluable tool.
It allows for the visualization of subtle changes in the brain and spinal cord that may not be apparent on other imaging modalities. The ability to visualize white matter lesions, a hallmark of MS, is particularly significant.
Role of MRI in MS Diagnosis
MRI plays a pivotal role in MS diagnosis by identifying characteristic lesions in the brain and spinal cord. These lesions are often associated with demyelination, a key pathological feature of MS. The presence of multiple lesions, both in space and time, is crucial for establishing a diagnosis. This means that lesions are found in different areas of the central nervous system, and that new lesions appear over time.
Key Features of MRI Scans Suggestive of MS
MRI scans suggestive of MS typically reveal multiple, well-defined lesions, often ovoid or rounded in shape. These lesions are frequently located in the periventricular white matter, the juxtacortical white matter, and the brainstem. Their appearance is often characterized by a hypointense signal on T1-weighted images and a hyperintense signal on T2-weighted images.
Significance of Lesions in MRI
The presence of lesions in MRI is crucial for MS diagnosis. These lesions are not only indicative of demyelination but also provide information about the disease’s extent and activity. The number, location, and characteristics of the lesions help clinicians assess the severity and progression of the disease. Furthermore, the presence of contrast enhancement in certain lesions can indicate active inflammation and disease activity.
Comparison of MRI Sequences
Different MRI sequences provide varying information about the lesions, making their combined use essential. These sequences differ in their sensitivity to various tissue properties, such as water content, fat content, and blood flow. This allows for a more comprehensive evaluation of the lesions and their characteristics.
Criteria for Lesion Detection and Characterization
The criteria for lesion detection and characterization involve meticulous analysis of MRI scans. Neurologists use standardized criteria to assess the presence, size, location, and characteristics of lesions. These criteria include the presence of at least one characteristic lesion, its location, and its appearance on different MRI sequences.
Location and Distribution of Lesions
The location and distribution of lesions in the brain and spinal cord are important diagnostic factors. Lesions in periventricular white matter, juxtacortical white matter, and brainstem are frequently observed in MS. The dissemination in space and time is vital for MS diagnosis, signifying that the lesions are distributed in multiple areas of the CNS and have been observed over time.
Table: MRI Sequences and Diagnostic Value
| MRI Sequence | Diagnostic Value |
|---|---|
| T1-weighted | Highlights areas of tissue loss or damage. Can be used to differentiate MS lesions from other conditions. |
| T2-weighted | Highlights areas of inflammation and water content. Highly sensitive to demyelination and is crucial in detecting MS lesions. |
| FLAIR (Fluid-attenuated inversion recovery) | Highlights demyelination and lesions by suppressing cerebrospinal fluid signals. Especially useful for visualizing lesions in the periventricular regions. |
| Contrast-enhanced | Highlights active inflammation. Used to identify areas of active disease and monitor disease progression. |
Neurological Examination
A thorough neurological examination is crucial in diagnosing multiple sclerosis (MS). It involves a systematic assessment of various neurological functions to identify potential signs and symptoms indicative of the disease. The examination should be tailored to the individual patient’s presentation and suspected areas of involvement. This assessment plays a pivotal role in determining the extent and pattern of neurological damage, supporting the clinical picture, and assisting in the differential diagnosis.
Essential Components of a Neurological Examination for MS
A comprehensive neurological examination for MS evaluates multiple areas, including mental status, cranial nerves, motor function, sensory function, coordination, reflexes, and gait. This multifaceted approach provides a holistic view of the patient’s neurological status, facilitating the identification of subtle signs that might be missed with a less detailed examination.
Assessing Neurological Functions in MS
Assessing neurological functions in MS requires careful observation and standardized testing procedures. For example, evaluating motor function involves assessing muscle strength, tone, and coordination. Sensory function is assessed by testing light touch, pain, temperature, and vibration perception. The evaluation of cranial nerves assesses specific functions like vision, hearing, and facial movement.
Importance of Specific Neurological Tests in MS
Specific neurological tests, such as the Romberg test, are crucial for identifying subtle signs of ataxia or balance problems, which can be indicative of MS. The assessment of deep tendon reflexes, and their presence or absence, can provide important information regarding potential demyelination.
Skills Required to Perform a Comprehensive Neurological Examination
Performing a comprehensive neurological examination requires specific skills, including knowledge of normal neurological function, the ability to accurately assess various neurological functions, and the capacity to interpret the results in the context of the patient’s clinical presentation. Thorough understanding of neurological anatomy and physiology is paramount. Careful documentation is also essential for accurate communication and follow-up.
Clinical Findings Indicative of MS
Clinical findings indicative of MS in a neurological examination can include abnormalities in muscle strength, coordination, sensation, reflexes, and cranial nerve function. For instance, an individual might exhibit weakness in one limb, difficulty with balance, or sensory changes in a specific area. These findings, when combined with other diagnostic criteria, can contribute significantly to the diagnosis.
Table: Key Aspects of a Neurological Examination Relevant to MS Diagnosis
| Neurological Function | Assessment Techniques | Potential MS Findings |
|---|---|---|
| Mental Status | Orientation, memory, attention, language | Mild cognitive impairment, difficulties with executive functions |
| Cranial Nerves | Visual acuity, pupillary reflexes, facial movements | Optic neuritis (visual impairment), facial weakness, double vision |
| Motor Function | Muscle strength, tone, coordination, reflexes | Weakness, spasticity, ataxia, hyperreflexia |
| Sensory Function | Light touch, pain, temperature, vibration | Sensory loss, paresthesia, dysesthesia |
| Coordination | Finger-to-nose test, heel-to-shin test | Dysmetria, intention tremor, ataxia |
| Reflexes | Biceps, triceps, brachioradialis, patellar, Achilles | Hyperreflexia, clonus, absent reflexes |
| Gait | Observe gait pattern, stance, and balance | Staggering gait, difficulty with turning, ataxia |
Diagnostic Criteria and Guidelines
Navigating the diagnostic journey for multiple sclerosis (MS) hinges on precise criteria. This isn’t a straightforward process; multiple factors must be considered to differentiate MS from other neurological conditions. Accurate diagnosis is critical for timely treatment and management.
Current Diagnostic Criteria
The most widely accepted and current diagnostic criteria for MS are the McDonald Criteria. These criteria, constantly evolving with new research, offer a more nuanced approach to diagnosis than previous versions. Their iterative nature reflects the ongoing pursuit of greater diagnostic precision.
Different Versions and Revisions
Several revisions of the McDonald Criteria have been published, each building upon the previous version to incorporate newer findings and enhance diagnostic accuracy. Early versions focused primarily on clinical presentation, while later versions incorporated imaging findings to improve diagnostic sensitivity and specificity. The revisions are crucial to ensure that diagnoses are more reliable and consistent across different healthcare settings.
Criteria for Different Types of MS
The McDonald Criteria differentiate between relapsing-remitting, primary-progressive, secondary-progressive, and progressive-relapsing MS. Each type presents distinct clinical characteristics, and the criteria account for these differences. For example, relapsing-remitting MS typically involves episodes of worsening symptoms followed by periods of remission, while primary-progressive MS involves a gradual worsening of symptoms from onset.
Distinguishing MS from Other Conditions
The criteria for distinguishing MS from other neurological conditions involve careful consideration of the patient’s medical history, neurological examination findings, and imaging results. A thorough evaluation is crucial to rule out other potential diagnoses, such as neuromyelitis optica spectrum disorder (NMOSD), stroke, or other inflammatory demyelinating disorders. The diagnostic process requires meticulous consideration of all potential factors.
Clinical Application of Diagnostic Criteria
The McDonald Criteria are used in clinical practice to establish a diagnosis of MS. Neurologists and other healthcare professionals utilize these criteria to evaluate patients with suspected MS. The criteria guide the diagnostic process, helping to determine if the clinical presentation aligns with the expected characteristics of MS. They are used in conjunction with a detailed patient history, neurological examination, and imaging studies to reach a comprehensive and accurate diagnosis.
Summary Table of Essential Diagnostic Criteria
| Criterion | Description | Example |
|---|---|---|
| Clinical Presentation | Evidence of MS lesions disseminated in space and time. | Episodes of optic neuritis, weakness in limbs, sensory disturbances. |
| Neurological Examination | Objective findings consistent with MS, such as deficits in motor, sensory, or cerebellar function. | Decreased reflexes, impaired coordination, visual field defects. |
| Magnetic Resonance Imaging (MRI) | Presence of characteristic lesions in the brain and spinal cord. | Multiple lesions with characteristic features (e.g., periventricular lesions, juxtacortical lesions). |
| Cerebrospinal Fluid (CSF) Analysis | Elevated immunoglobulin G (IgG) oligoclonal bands in the CSF. | Presence of oligoclonal bands in the CSF not typical of other disorders. |
| Exclusion of Other Disorders | Rule out other conditions that mimic MS. | Thorough investigation to eliminate other diagnoses, including vascular lesions. |
“The McDonald Criteria represent a crucial tool in the diagnostic process, allowing for a more accurate and consistent identification of multiple sclerosis.”
Figuring out multiple sclerosis diagnostic criteria can be tricky, involving a combination of neurological exams and medical history review. It’s important to remember that support groups, like ask an expert hiv support groups , can be incredibly helpful in navigating the complexities of a diagnosis. Ultimately, understanding the diagnostic criteria is key to effective management of multiple sclerosis.
Differential Diagnosis
Pinpointing the exact cause of neurological symptoms is crucial for appropriate treatment. Multiple sclerosis (MS) can mimic various other neurological disorders, making a precise diagnosis challenging. Accurately differentiating MS from these conditions is essential for effective management and to avoid potentially harmful misdiagnosis. A comprehensive differential diagnosis process involves careful evaluation of symptoms, medical history, and diagnostic tests.
Conditions Mimicking MS
Numerous neurological conditions can present with symptoms similar to MS, necessitating a thorough evaluation to rule them out. These conditions often share overlapping clinical features, such as neurological deficits and inflammatory responses. Careful attention to subtle differences in symptom presentation and progression is essential.
- Neuropathies: Conditions affecting the peripheral nerves, such as Guillain-Barré syndrome, chronic inflammatory demyelinating polyneuropathy (CIDP), and other types of mononeuropathies, can cause weakness, numbness, and pain that mimic MS symptoms. Differentiating these conditions involves examining the pattern of nerve involvement and the presence of specific antibodies.
- Vascular Disorders: Strokes, transient ischemic attacks (TIAs), and other vascular events can result in neurological symptoms that overlap with MS. Careful assessment of the patient’s risk factors, such as hypertension and hyperlipidemia, and the pattern of symptom onset and progression helps distinguish vascular disorders from MS. Neuroimaging plays a critical role in evaluating vascular involvement.
- Infections: Certain infections, such as Lyme disease, HIV, and neurosarcoidosis, can manifest with neurological symptoms that mimic MS. Evaluating the presence of specific antibodies or other markers associated with these infections is crucial for distinguishing them from MS.
- Demyelinating Disorders: Other demyelinating disorders, such as neuromyelitis optica spectrum disorder (NMOSD), can have similar symptoms to MS. NMOSD is characterized by a more specific pattern of lesions involving the optic nerves and spinal cord. Differentiating these disorders often relies on the results of MRI scans, cerebrospinal fluid (CSF) analysis, and specific antibody testing.
- Tumors: Brain tumors or spinal cord tumors can cause neurological deficits that mimic MS. Neuroimaging techniques, such as MRI, are critical for identifying the presence and location of tumors.
- Multiple System Atrophy (MSA): MSA is a progressive neurodegenerative disorder that can present with parkinsonian features and cerebellar signs that mimic MS. Differentiating MS from MSA often relies on the progressive nature of the symptoms and the absence of typical MS-associated symptoms.
Importance of Thorough Differential Diagnosis
A comprehensive differential diagnosis is crucial for ensuring accurate diagnosis and appropriate management. Misdiagnosis can lead to ineffective or even harmful treatments, delaying or preventing effective interventions. Ruling out other conditions is critical for providing the most effective care.
Navigating multiple sclerosis diagnostic criteria can be tricky, often involving a range of symptoms. One such symptom, that can sometimes feel surprisingly intertwined with MS, is the fear of intimacy. Understanding the causes and treatments for this, like exploring fear of intimacy symptoms causes treatment , can offer a more complete picture of the patient experience. Ultimately, accurately pinpointing multiple sclerosis diagnostic criteria remains a crucial first step in effective treatment.
Steps for Distinguishing MS from Similar Conditions
A systematic approach is necessary to distinguish MS from other neurological conditions. This involves a multi-step process, including a detailed patient history, thorough neurological examination, and appropriate diagnostic tests.
- Comprehensive Medical History: Gathering a detailed medical history, including prior illnesses, family history, and any relevant exposures, is critical to identify potential risk factors and patterns of symptom onset.
- Neurological Examination: A detailed neurological examination, including assessment of motor skills, sensory functions, coordination, and reflexes, helps identify specific patterns of neurological dysfunction.
- Diagnostic Tests: Diagnostic tests, such as MRI scans, evoked potentials, and CSF analysis, can provide critical information about the presence of demyelinating lesions and inflammatory processes.
- Imaging Techniques: MRI is essential for visualizing brain and spinal cord lesions. The pattern, location, and timing of lesions aid in differentiating MS from other conditions.
Significance of Ruling Out Other Diagnoses
Accurate diagnosis is paramount for effective treatment and management. Avoiding misdiagnosis can prevent unnecessary treatments, provide appropriate interventions, and ensure the best possible outcome for patients. Correctly identifying and excluding alternative diagnoses ensures the patient receives the most effective care tailored to their specific condition.
Comparison Table, Multiple sclerosis diagnostic criteria
| Characteristic | Multiple Sclerosis | Guillain-Barré Syndrome | Stroke | Brain Tumor |
|---|---|---|---|---|
| Symptoms | Variable, including numbness, weakness, vision problems, fatigue | Progressive muscle weakness, often starting in the legs | Sudden onset of neurological deficits, often affecting one side of the body | Gradual or sudden onset of neurological deficits, depending on tumor location |
| Imaging Findings | Multiple, disseminated white matter lesions in brain and spinal cord | Often normal or shows minor findings | Focal brain or spinal cord lesions, often with vascular abnormalities | Mass lesion on MRI |
| CSF Analysis | May show elevated IgG index and oligoclonal bands | Often normal or shows minor findings | May show abnormalities related to vascular injury | May show abnormalities depending on the tumor type |
Supporting Information and Considerations
Navigating the complexities of Multiple Sclerosis (MS) diagnosis requires a multifaceted approach. Beyond the core diagnostic criteria, a wealth of supporting information can significantly inform the process. Understanding patient history, environmental influences, and potential comorbidities is crucial for a comprehensive assessment. This section delves into these supporting elements and highlights the significance of a multidisciplinary approach to MS care.
Patient History and Family History
Patient history plays a vital role in MS diagnosis. A detailed account of symptom onset, progression, and associated factors like stress, infections, or lifestyle changes can offer crucial insights. Similarly, a thorough family history, including any instances of neurological disorders, can help assess genetic predisposition. For example, individuals with a family history of MS might require more vigilant monitoring and earlier intervention.
Recognizing these factors can aid in developing an individualized treatment strategy.
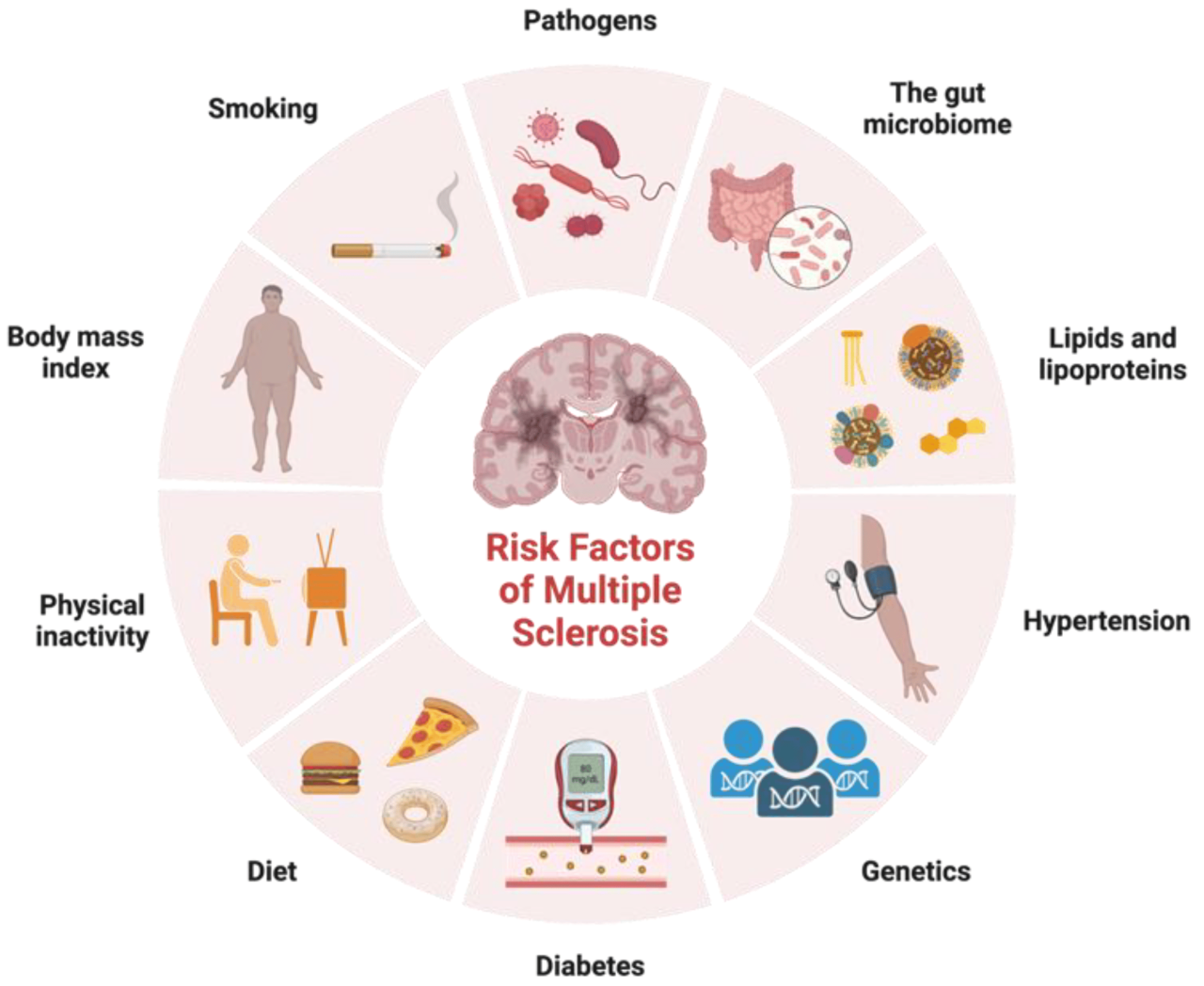
Environmental Factors
Environmental factors can influence MS development, though the precise mechanisms remain complex. Studies have suggested a correlation between certain infections, vitamin D levels, and geographic location with MS risk. For example, individuals living in areas with lower sunlight exposure might have a higher risk of vitamin D deficiency, a potential factor in MS development.
Significance of Other Medical Conditions
Co-existing medical conditions can potentially impact MS diagnosis and management. Symptoms of other neurological disorders can mimic MS symptoms, necessitating a thorough differential diagnosis. Accurate identification of underlying conditions is essential to ensure appropriate treatment. For example, some symptoms of migraine, like vision problems, can be confused with optic neuritis, a common MS symptom.
Multidisciplinary Approaches
A multidisciplinary approach is paramount in the management of MS. Neurologists, neuropsychologists, physical therapists, occupational therapists, and social workers often collaborate to provide holistic care. This collaborative approach addresses the diverse needs of individuals with MS, including physical, cognitive, and emotional aspects.
Potential Contributing Factors in MS Diagnosis
| Category | Factors | Explanation |
|---|---|---|
| Genetic Predisposition | Family history of MS, specific genetic variations | Family history of neurological disorders significantly increases the risk. Certain genes may increase susceptibility. |
| Environmental Factors | Infections (e.g., Epstein-Barr virus), vitamin D deficiency, geographic location, smoking | Exposure to certain pathogens, low vitamin D levels, and location can be risk factors. Smoking has also been linked to increased risk. |
| Lifestyle Factors | Diet, stress levels, physical activity | Healthy lifestyle choices, including a balanced diet and regular exercise, can potentially influence the course of MS. Stress management is crucial for well-being. |
| Co-existing Conditions | Migraines, infections, other autoimmune disorders | Co-occurring conditions may mimic MS symptoms or complicate management. |
| Diagnostic Inconsistencies | Variability in symptom presentation, difficulty in distinguishing from other neurological conditions | Symptoms may vary considerably between individuals, making diagnosis challenging. |
End of Discussion
In conclusion, the diagnostic journey for multiple sclerosis involves a combination of clinical assessments, laboratory tests, and imaging techniques. A thorough understanding of the diagnostic criteria, coupled with a detailed patient history and neurological examination, plays a critical role in distinguishing MS from other neurological conditions. This comprehensive guide provides a valuable resource for healthcare professionals and those seeking to better understand the process of diagnosing multiple sclerosis.

Leave a Reply