Hypoglycemia causes risk factors are a crucial area of study, impacting many individuals. This exploration delves into the multifaceted causes and risks associated with low blood sugar. Understanding the mechanisms behind hypoglycemia, from normal blood glucose regulation to the impact of various diseases, medications, and lifestyle choices, is paramount. This comprehensive guide explores the complex interplay of risk factors, empowering readers with knowledge to proactively manage and prevent this potentially serious condition.
This article will discuss the intricate interplay of genetics, medication side effects, dietary habits, physical activity, and stress levels on the development and progression of hypoglycemia. We’ll examine the role of various medical conditions in causing hypoglycemia, highlighting specific risk factors for each. Furthermore, we’ll delve into the importance of timely diagnosis, effective prevention strategies, and the management of hypoglycemia episodes.
The long-term complications and the importance of early intervention will also be addressed.
Introduction to Hypoglycemia
Hypoglycemia, or low blood sugar, occurs when the level of glucose in the blood falls below the normal range. This condition can range from mild discomfort to severe complications, potentially threatening life. Understanding the mechanisms behind hypoglycemia and the normal regulation of blood glucose is crucial for prevention and management. This section will delve into the physiological underpinnings of hypoglycemia, highlighting the delicate balance involved in maintaining healthy blood sugar levels.The body tightly regulates blood glucose levels through a complex interplay of hormones and metabolic pathways.
This intricate system ensures a consistent supply of energy to the body’s cells, particularly the brain. Disruptions in this process can lead to hypoglycemia, impacting various bodily functions. We will explore the normal blood glucose regulation process and different types of hypoglycemia, emphasizing their causes and characteristics.
Definition of Hypoglycemia
Hypoglycemia is defined as a blood glucose level below the normal range, typically below 70 mg/dL (3.9 mmol/L). This low glucose concentration can lead to a variety of symptoms, depending on the severity and the rate of decline. Early symptoms may include shakiness, sweating, and anxiety, while more severe cases can result in confusion, seizures, and loss of consciousness.
Physiological Mechanisms of Hypoglycemia
The body maintains blood glucose levels through a complex interplay of hormones, primarily insulin and glucagon. Insulin promotes glucose uptake by cells, while glucagon stimulates the liver to release stored glucose. Disruptions in this balance, either due to excessive insulin production or insufficient glucose production, can lead to hypoglycemia. Other factors, such as impaired liver function, hormonal imbalances, or certain medications, can also contribute.
Normal Blood Glucose Regulation
The body maintains a tight regulation of blood glucose through a feedback loop involving several hormones and organs. The pancreas, in response to rising glucose levels, secretes insulin, which facilitates the uptake of glucose into cells. Conversely, when glucose levels fall, the pancreas secretes glucagon, prompting the liver to release stored glucose into the bloodstream. The liver also plays a vital role in producing glucose through gluconeogenesis, a process of synthesizing glucose from non-carbohydrate sources.
The adrenal medulla also secretes epinephrine, which further promotes glucose release. This coordinated action of hormones and organs ensures a constant supply of glucose for energy needs.
Types of Hypoglycemia
The following table categorizes various types of hypoglycemia, highlighting their defining characteristics:
| Type of Hypoglycemia | Defining Characteristics | Common Causes |
|---|---|---|
| Reactive Hypoglycemia | Occurs after a meal, typically in individuals with impaired glucose tolerance or certain gastrointestinal conditions. | Rapid absorption of sugars, impaired insulin secretion after meals, gastrointestinal issues. |
| Fasting Hypoglycemia | Occurs in the absence of food intake, typically due to excessive insulin production or impaired glucose production by the liver. | Insulinoma, certain medications, adrenal insufficiency, liver disease. |
| Postprandial Hypoglycemia | Occurs after a meal, a form of reactive hypoglycemia. | Increased insulin sensitivity, certain medications, pancreatic disorders. |
| Drug-Induced Hypoglycemia | Occurs as a side effect of certain medications, including some diabetes medications and other drugs. | Certain diabetes medications, alcohol, certain beta-blockers. |
Underlying Causes of Hypoglycemia
Hypoglycemia, or low blood sugar, is a potentially serious condition that requires prompt medical attention. Understanding the underlying causes of hypoglycemia is crucial for diagnosis and effective management. This involves recognizing the diverse range of factors that can disrupt the delicate balance of blood glucose regulation, from underlying diseases to medication interactions. This exploration will delve into the mechanisms and risk factors associated with various causes, providing a comprehensive overview of this complex condition.
Common Causes of Hypoglycemia Categorized by Disease or Condition
A variety of medical conditions can disrupt the body’s ability to maintain normal blood sugar levels, leading to hypoglycemia. The following table categorizes common causes based on the underlying disease or condition.
| Disease/Condition | Mechanism of Hypoglycemia | Risk Factors |
|---|---|---|
| Diabetes Mellitus (Type 1 and Type 2) | In type 1 diabetes, the body doesn’t produce insulin, leading to elevated blood glucose levels. If insulin is administered, or the individual has taken too much insulin, blood glucose levels can fall below normal. In type 2 diabetes, insulin resistance can cause fluctuating blood sugar levels that can sometimes fall too low, especially when combined with insulin or other hypoglycemic medications. | Missed or inadequate meals, strenuous exercise, alcohol consumption, changes in insulin dose or timing, or infections. For type 2, often related to inadequate lifestyle changes. |
| Pancreatic Insufficiency | Conditions like pancreatitis or cystic fibrosis can impair the pancreas’s ability to produce and release hormones like insulin, resulting in hypoglycemia. | History of pancreatic diseases, genetic predisposition, or certain medications. |
| Adrenal Insufficiency | Adrenal glands produce hormones that regulate blood sugar. If the adrenal glands don’t produce enough of these hormones, it can cause hypoglycemia. | Genetic predisposition, autoimmune disorders, or infections. |
| Liver Disease | The liver plays a critical role in maintaining blood glucose levels. Damage or dysfunction of the liver can disrupt this process, potentially leading to hypoglycemia. | Chronic alcohol abuse, hepatitis, cirrhosis, or certain medications. |
| Certain Tumors | Rarely, tumors in the pancreas or other parts of the body can produce excessive insulin, leading to hypoglycemia. | Age, family history of tumors, or exposure to certain toxins. |
Mechanisms of Hypoglycemia, Hypoglycemia causes risk factors
Understanding the underlying mechanisms by which various causes lead to hypoglycemia is essential for developing targeted interventions. The mechanisms can range from a deficiency in glucose production to an overproduction or inappropriate use of insulin.
- Diabetes Mellitus: In type 1 diabetes, the lack of insulin prevents the body from using glucose for energy. In type 2 diabetes, insulin resistance means the body doesn’t respond properly to insulin, which can cause elevated blood sugar, and in some cases, if there’s an overcorrection with medication, it can drop below normal.
- Pancreatic Insufficiency: The pancreas’s failure to produce enough insulin directly leads to inadequate glucose uptake by cells, resulting in low blood sugar.
- Adrenal Insufficiency: A deficiency in hormones produced by the adrenal glands can disrupt the body’s ability to regulate blood glucose levels, potentially causing hypoglycemia.
- Liver Disease: The liver’s role in glucose production is critical. Liver damage or dysfunction impairs this process, resulting in insufficient glucose release into the bloodstream, leading to hypoglycemia.
- Tumors: Certain tumors can produce excessive insulin or other substances that mimic its effects, leading to hypoglycemia.
Risk Factors Associated with Different Causes
Risk factors for hypoglycemia vary depending on the underlying cause. Identifying these factors can help in proactive management and prevention.
- Diabetes Mellitus: Missed or inadequate meals, strenuous exercise, alcohol consumption, and changes in insulin dose or timing are common risk factors for hypoglycemia in individuals with diabetes.
- Pancreatic Insufficiency: Risk factors include a history of pancreatic diseases, genetic predisposition, and certain medications.
- Adrenal Insufficiency: Genetic predisposition, autoimmune disorders, and infections can contribute to the risk of hypoglycemia.
- Liver Disease: Chronic alcohol abuse, hepatitis, cirrhosis, and certain medications are potential risk factors for hypoglycemia associated with liver conditions.
- Tumors: Age, family history of tumors, and exposure to certain toxins may increase the risk of hypoglycemia associated with tumor growth.
Role of Genetics in Hypoglycemia
Genetic factors play a role in predisposing individuals to certain types of hypoglycemia. Some individuals may inherit a predisposition to conditions that increase the risk of developing the condition.
Role of Medication in Causing Hypoglycemia
Many medications can inadvertently cause hypoglycemia. Careful monitoring and adjustments to medication regimens are crucial in managing this risk.
Common Medications Leading to Hypoglycemia
Several medications, particularly those used to treat diabetes or other conditions, can contribute to hypoglycemia.
Understanding hypoglycemia risk factors is crucial for preventative measures. While factors like poor diet and insufficient insulin can play a role, a healthy immune system is equally important. This is why recommended vaccinations for healthcare workers are so vital in preventing infectious diseases that can exacerbate hypoglycemia risk. Ultimately, maintaining overall health through proper nutrition and a strong immune system are key to managing hypoglycemia effectively.
| Drug Class | Examples |
|---|---|
| Insulin | Regular insulin, NPH insulin, Lispro insulin |
| Sulfonylureas | Glipizide, Glyburide |
| Meglitinides | Repaglinide, Nateglinide |
| Certain Anti-diabetic medications | Acarbose, Miglitol, Metformin |
Risk Factors for Hypoglycemia
Understanding the factors that increase the risk of hypoglycemia is crucial for prevention and management. Identifying these triggers allows individuals to take proactive steps to mitigate their risk and maintain healthy blood sugar levels. This section delves into modifiable and non-modifiable risk factors, exploring their impact on hypoglycemia susceptibility.
Modifiable Risk Factors
Several lifestyle choices and habits can significantly influence the risk of developing hypoglycemia. Addressing these factors can often lead to a substantial reduction in the likelihood of experiencing episodes.
- Dietary Habits: Inadequate or erratic carbohydrate intake can disrupt blood sugar regulation, making individuals more vulnerable to hypoglycemia. Skipping meals or consuming excessive amounts of simple sugars followed by periods of low carbohydrate intake can create fluctuations in blood glucose levels. Examples include consuming sugary drinks, or consuming large portions of sugary snacks or meals followed by a prolonged period of time without consuming any carbohydrates.
Conversely, consistently low carbohydrate intake, particularly in individuals with diabetes, can also lead to hypoglycemia.
- Physical Activity: Exercise, while generally beneficial, can sometimes trigger hypoglycemia, especially if not managed appropriately. Intense or prolonged physical activity can deplete blood sugar stores, leading to a sudden drop in blood glucose levels. This is particularly true for individuals with diabetes, especially if their medication regimen isn’t adjusted to account for the activity level. For instance, an individual taking insulin may need to adjust their dose before engaging in vigorous exercise to prevent a hypoglycemic episode.
- Stress Levels: Stress can significantly impact blood sugar control. Hormones released during stressful situations can disrupt the delicate balance of blood sugar, potentially leading to hypoglycemia. Chronic stress can have a cumulative effect on blood glucose levels and can further increase the risk of experiencing episodes.
- Medication Use: Certain medications, including those used to treat diabetes or other conditions, can interact with the body’s natural blood sugar regulation processes and increase the risk of hypoglycemia. For example, taking insulin or other diabetes medications without adhering to a consistent meal plan can trigger a significant drop in blood glucose levels.
Age and Sex as Risk Factors
Age and sex can play a role in hypoglycemia risk, although the exact mechanisms are not fully understood.
While age-related changes in metabolism can influence blood sugar regulation, there’s no definitive evidence to link age directly to an increased risk of hypoglycemia. The impact of sex hormones on blood sugar balance might also play a role in varying levels of risk between men and women, but more research is needed to understand this connection fully.
Lifestyle Choices and Hypoglycemia Risk
Maintaining a consistent lifestyle, including regular meals, adequate sleep, and stress management techniques, can significantly reduce the risk of hypoglycemia.
Consistent routines in daily life, such as meal timing and exercise schedules, can help stabilize blood glucose levels. Adequate sleep is also essential, as sleep deprivation can disrupt hormonal balances and affect blood sugar control. Effective stress management techniques, such as mindfulness and relaxation exercises, can help mitigate the impact of stress on blood sugar regulation. Individuals can benefit from creating a routine that supports stable blood glucose levels.
Dietary Habits and Hypoglycemia Risk
Certain dietary habits can increase the risk of hypoglycemia. Consistent consumption of refined carbohydrates or large amounts of simple sugars can cause blood glucose levels to spike and then subsequently crash, resulting in hypoglycemic episodes.
A diet rich in refined carbohydrates can cause a rapid rise in blood sugar followed by a sharp drop, increasing the likelihood of experiencing hypoglycemia. Conversely, a balanced diet with adequate protein and fiber can help regulate blood glucose levels and prevent fluctuations. Examples include consuming large amounts of processed foods, sugary drinks, or skipping meals. A diet rich in complex carbohydrates, fruits, vegetables, and lean proteins can help maintain stable blood glucose levels.
Physical Activity and Hypoglycemia Risk
The intensity and duration of physical activity can impact blood sugar levels. Individuals who engage in prolonged or intense exercise without proper adjustments to their diet or medication may experience hypoglycemia.
Engaging in prolonged or strenuous physical activity without proper carbohydrate intake can lead to a rapid drop in blood sugar levels, triggering hypoglycemia. Individuals should carefully monitor their blood sugar levels before, during, and after exercise, especially if they have diabetes or are taking medication that affects blood sugar control. For instance, athletes or individuals participating in intense training regimens should consider adjusting their carbohydrate intake to prevent episodes of hypoglycemia.
Stress and Hypoglycemia
Stressful situations can trigger hormonal changes that affect blood sugar regulation. Chronic stress can contribute to a higher risk of hypoglycemia.
The body’s response to stress involves the release of hormones like cortisol, which can elevate blood sugar levels. However, chronic or prolonged stress can disrupt the body’s ability to regulate blood sugar, potentially leading to hypoglycemia. Stress management techniques, including relaxation exercises and mindfulness practices, can help mitigate the impact of stress on blood sugar control.
Interaction of Multiple Risk Factors
| Risk Factor | Potential Impact on Hypoglycemia | Example |
|---|---|---|
| Inadequate Carbohydrate Intake | Blood sugar drops too low | Skipping meals or consuming a very low carbohydrate diet |
| Intense Physical Activity | Blood sugar drops during or after exercise | Long-duration intense workout without adequate carbohydrate intake |
| Stress | Disruption of blood sugar regulation | Experiencing prolonged periods of stress or anxiety |
| Medication Interaction | Blood sugar drops due to medication effects | Taking insulin without adjusting for activity levels |
Symptoms and Diagnosis of Hypoglycemia
Recognizing the signs of hypoglycemia is crucial for prompt treatment and preventing serious complications. Understanding the spectrum of symptoms, from mild to severe, empowers individuals and healthcare providers to intervene effectively. Accurate diagnosis relies on a combination of symptom evaluation and blood glucose testing.Hypoglycemia, or low blood sugar, manifests in a range of symptoms, often varying in intensity depending on the severity and speed of the drop in blood glucose levels.
Early detection and intervention are paramount to preventing severe consequences.
Common Symptoms of Hypoglycemia
Early symptoms often begin subtly, progressing to more pronounced signs as blood sugar levels continue to decrease. Recognizing these early warning signs is vital for preventing severe episodes.
- Mild symptoms typically include shakiness, sweating, anxiety, hunger, and dizziness. These initial symptoms often signal a need to raise blood sugar levels quickly.
- As hypoglycemia progresses, symptoms can escalate to include confusion, difficulty concentrating, blurred vision, headache, and slurred speech. These symptoms indicate a more significant drop in blood glucose and warrant immediate intervention.
- Severe hypoglycemia can lead to loss of consciousness, seizures, and coma. This is a medical emergency requiring immediate attention and typically involves the administration of glucose intravenously.
Differentiating Mild and Severe Hypoglycemia
A clear understanding of the differences between mild and severe hypoglycemic symptoms is essential for timely intervention. Prompt recognition and appropriate action can prevent progression to more serious complications.
| Symptom Category | Mild Symptoms | Severe Symptoms |
|---|---|---|
| Physical Symptoms | Shakiness, sweating, anxiety, hunger, dizziness, lightheadedness, palpitations | Confusion, difficulty concentrating, slurred speech, blurred vision, headache, loss of coordination, seizures, loss of consciousness, coma |
| Mental Symptoms | Irritability, nervousness, difficulty with focus, feeling tired, numbness around the mouth | Inappropriate behavior, hallucinations, memory loss, difficulty speaking, lack of responsiveness, loss of consciousness |
| Treatment | Consume a fast-acting carbohydrate (e.g., juice, glucose tablets) and monitor blood sugar | Seek immediate medical attention. Intravenous glucose administration may be required. |
Diagnostic Process for Hypoglycemia
Accurate diagnosis involves a combination of symptom evaluation and blood glucose testing. This process ensures prompt intervention to prevent complications.A comprehensive evaluation begins with a thorough assessment of the patient’s medical history and symptoms. Blood glucose testing plays a critical role in confirming the diagnosis.
Blood glucose testing provides a quantitative measure of the blood sugar level, enabling clinicians to determine the severity of the hypoglycemic episode.
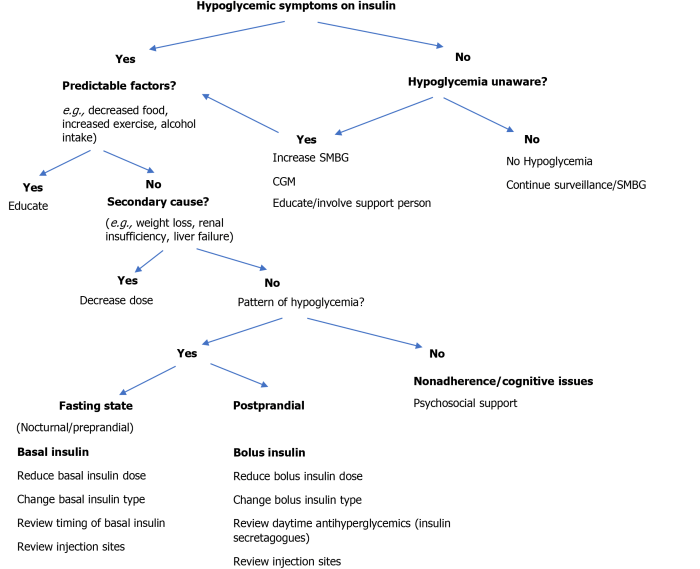
Role of Continuous Glucose Monitoring (CGM)
Continuous glucose monitoring (CGM) systems offer real-time insights into blood glucose fluctuations, providing valuable information for both diagnosis and management of hypoglycemia. These systems can detect trends and patterns in glucose levels, which are often missed with traditional blood glucose testing.CGM systems offer a continuous stream of data, enabling the detection of subtle drops in blood sugar that might otherwise go unnoticed.
This continuous monitoring allows for more proactive management and potentially prevents severe hypoglycemic episodes.
Importance of Timely Diagnosis
Early diagnosis and treatment of hypoglycemia are critical to preventing potentially serious complications. Prolonged episodes of low blood sugar can cause irreversible damage to various organs.Delaying treatment can lead to a cascade of negative consequences, including permanent neurological damage, coma, and even death. Early intervention is key to mitigating these risks.
Prevention and Management Strategies
Managing hypoglycemia effectively involves a proactive approach that combines consistent lifestyle choices with prompt responses to episodes. By understanding the triggers and implementing preventive measures, individuals can significantly reduce the frequency and severity of hypoglycemic events. A structured approach to managing episodes, combined with education and awareness, is crucial for maintaining overall well-being.
Preventive Measures to Reduce Hypoglycemia Risk
Consistent lifestyle choices are essential in preventing hypoglycemia. A well-structured daily routine that incorporates regular meals and snacks can help regulate blood sugar levels. This approach ensures a consistent supply of glucose to the body, preventing sudden drops. Avoiding excessive alcohol consumption and regular exercise also play a key role in maintaining stable blood sugar levels.
- Regular Meals and Snacks: Maintaining a consistent meal schedule, including regular snacks, helps to prevent blood sugar from dipping too low. Skipping meals or eating irregularly can lead to unpredictable blood sugar fluctuations.
- Balanced Diet: Choosing a balanced diet that includes complex carbohydrates, lean proteins, and healthy fats can contribute to more stable blood sugar levels over time. Avoid simple sugars as they can cause rapid spikes and subsequent drops.
- Avoid or Limit Alcohol Consumption: Alcohol can impair the body’s ability to regulate blood sugar, increasing the risk of hypoglycemia, especially in individuals with pre-existing conditions.
- Regular Exercise: While exercise can improve overall health and well-being, it’s important to understand how it impacts blood sugar levels. Individuals with conditions that affect blood sugar regulation need to monitor their blood sugar levels before, during, and after exercise to adjust their intake of carbohydrates accordingly.
- Stress Management: Stress can sometimes affect blood sugar levels. Practicing stress-reducing techniques like meditation, yoga, or deep breathing exercises can be helpful in managing these effects.
Importance of Maintaining a Consistent Meal Schedule
A consistent meal schedule is crucial for regulating blood sugar levels. The body relies on a predictable intake of glucose for energy, and irregular eating patterns can disrupt this process, potentially leading to hypoglycemia. Predictable meals provide a steady supply of glucose, helping to prevent sudden drops.
Role of Regular Blood Glucose Monitoring in Prevention
Regular blood glucose monitoring is a vital tool for preventing hypoglycemia. By tracking blood sugar levels throughout the day, individuals can identify patterns and adjust their meal plans or medication accordingly. This proactive approach allows for early intervention and prevents severe episodes.
- Early Detection: Regular monitoring allows for early detection of potential hypoglycemic trends, enabling individuals to adjust their actions to prevent a more serious drop in blood sugar levels.
- Pattern Recognition: Monitoring blood sugar levels over time can help identify patterns in blood sugar fluctuations, such as those related to specific meals, activities, or medications. This information is critical in identifying potential triggers for hypoglycemia.
- Personalized Adjustments: Individuals can use monitoring data to make personalized adjustments to their diet, exercise routines, or medication schedules to maintain healthy blood sugar levels.
Managing Hypoglycemia Episodes
Developing a plan for managing hypoglycemia episodes is crucial. Having a rapid-acting glucose source readily available can significantly lessen the impact of an episode. This plan should also include knowing when to seek immediate medical attention.
- Rapid-Acting Glucose Sources: Having easily accessible rapid-acting glucose sources, such as glucose tablets, gels, or juice, is essential for quickly raising blood sugar levels during a hypoglycemic episode. Knowing the appropriate amount to consume based on individual needs is critical.
- Medical Assistance: Understanding when to seek immediate medical attention is vital. Severe or prolonged hypoglycemia can be life-threatening. Familiarize yourself with the symptoms that require immediate medical intervention.
Use of Rapid-Acting Glucose Sources
Rapid-acting glucose sources, like glucose tablets or gels, are designed to quickly raise blood sugar levels. These sources provide a concentrated dose of glucose, allowing for a faster recovery from hypoglycemia. Careful consideration of the appropriate dosage is essential to avoid overcorrection.
Using the correct amount of rapid-acting glucose is crucial. Too much can lead to hyperglycemia, a condition of elevated blood sugar.
Importance of Educating Individuals About Hypoglycemia
Education about hypoglycemia is paramount. Understanding the causes, symptoms, and management strategies is essential for effective self-management. This empowers individuals to take control of their health and prevent potentially serious consequences.
- Self-Management: Education empowers individuals to become active participants in their health management. This includes recognizing the early warning signs of hypoglycemia and taking appropriate action.
- Early Intervention: Education enables individuals to respond promptly to hypoglycemia episodes, preventing severe complications.
Effective Management Strategies Summary
| Strategy | Description |
|---|---|
| Consistent Meal Schedule | Maintaining regular meals and snacks to regulate blood sugar levels. |
| Blood Glucose Monitoring | Tracking blood sugar levels to identify patterns and adjust treatment plans. |
| Rapid-Acting Glucose Sources | Having readily available sources (e.g., glucose tablets, gels) for quick blood sugar elevation during episodes. |
| Education and Awareness | Understanding the causes, symptoms, and management of hypoglycemia. |
Long-Term Complications of Hypoglycemia
Hypoglycemia, while often a manageable condition, can lead to significant long-term complications if left untreated or poorly controlled. Understanding these potential consequences is crucial for individuals with diabetes and their healthcare providers to ensure proactive management and minimize risks. Early recognition and intervention are key to mitigating the impact of these complications.
Impact on Cognitive Function
Hypoglycemia can significantly affect cognitive function, potentially leading to a range of problems. Reduced blood sugar levels can impair brain function, affecting concentration, memory, and decision-making. Individuals experiencing frequent or severe hypoglycemia may experience symptoms such as confusion, difficulty concentrating, or even loss of consciousness. The severity of these cognitive impairments varies greatly depending on the frequency, duration, and severity of the hypoglycemic events.
Link Between Recurrent Hypoglycemia and Neurological Damage
Repeated episodes of hypoglycemia can potentially lead to neurological damage. Prolonged periods of low blood sugar can deprive the brain of essential glucose, leading to neuronal dysfunction and potentially irreversible damage. This damage can manifest as various neurological problems, including memory loss, cognitive decline, and even seizures. The cumulative effect of recurrent hypoglycemia over time can significantly increase the risk of long-term neurological complications.
Potential Cardiovascular Complications
While less frequently discussed, hypoglycemia can also have a detrimental impact on cardiovascular health. Studies suggest a correlation between recurrent hypoglycemia and an increased risk of cardiovascular events. The body’s response to hypoglycemia can involve the release of stress hormones, which can strain the cardiovascular system. This chronic stress can contribute to hypertension, abnormal heart rhythms, and an increased risk of heart attack or stroke.
Understanding hypoglycemia’s risk factors is crucial for prevention. While various factors contribute, a recent study on the impact of seed oils on inflammation and diabetes risk ( seed oils lower inflammation and diabetes risk study ) suggests a potential link. Further research is needed to fully grasp how dietary changes might influence hypoglycemia risk factors, but it’s clear that a holistic approach, considering both lifestyle and potential dietary influences, is key.
Importance of Early Intervention
Early intervention is crucial in preventing the long-term complications of hypoglycemia. Prompt recognition and treatment of hypoglycemic episodes are essential to minimize the damage to the brain and other organs. Regular monitoring of blood glucose levels, adherence to treatment plans, and appropriate management strategies are all vital in preventing the onset of these complications.
So, hypoglycemia, or low blood sugar, has a few key causes and risk factors. For example, skipping meals can definitely contribute, as can certain medications. And while coughing after running in cold weather might seem unrelated , it’s a good reminder to always be mindful of how your body reacts to different situations. Poorly managed diabetes or certain underlying health conditions can also play a role in hypoglycemia risk factors.
Relationship Between Severity and Frequency of Hypoglycemia and Risk of Long-Term Complications
The severity and frequency of hypoglycemic episodes directly correlate with the risk of long-term complications. More frequent and severe episodes expose the body to greater periods of low blood sugar, increasing the risk of neurological damage, cognitive impairment, and cardiovascular problems. Individuals experiencing frequent and severe hypoglycemia should closely monitor their blood sugar levels and discuss any concerns with their healthcare provider.
Correlation Between Hypoglycemia and Specific Complications
| Hypoglycemia Feature | Potential Complications |
|---|---|
| Frequent, Severe Hypoglycemic Episodes | Increased risk of cognitive decline, neurological damage (e.g., memory loss, dementia), and cardiovascular events (e.g., heart attack, stroke). |
| Unrecognized or Untreated Hypoglycemia | Potentially severe or irreversible neurological damage, coma, and death. |
| Inadequate Blood Glucose Control | Increased likelihood of all hypoglycemia-related complications, particularly with prolonged duration. |
| Inability to Recognize Symptoms | Increased risk of severe hypoglycemia and related complications, as individuals may not seek prompt treatment. |
Illustrative Examples
Understanding hypoglycemia requires exploring real-world scenarios. This section provides detailed examples to illustrate how various factors contribute to this condition, highlighting the importance of proactive prevention and effective management. We’ll delve into specific medical conditions, medications, lifestyle choices, and dietary patterns to demonstrate their impact on blood glucose levels.
A Case of Insulin-Induced Hypoglycemia
Insulin is a crucial hormone for regulating blood sugar. However, an overdose or improper timing of insulin injections can lead to dangerously low blood sugar. For example, a patient with type 1 diabetes taking insulin for blood sugar control might experience hypoglycemia if they take a larger dose than prescribed or if they skip a meal after an injection.
The body’s inability to produce enough glucose to counter the insulin’s effect results in a rapid drop in blood sugar. Symptoms such as shakiness, sweating, and confusion can arise. Prompt treatment with glucose tablets or a sugary drink is vital to restore normal blood sugar levels.
Medication Impact on Blood Glucose
Certain medications can either directly or indirectly affect blood sugar. Beta-blockers, commonly used to treat high blood pressure, can mask the classic symptoms of hypoglycemia. This masking effect makes it difficult for patients to recognize a hypoglycemic event. Consequently, the patient may not receive prompt treatment, leading to more severe complications. Additionally, some medications, like corticosteroids, can raise blood sugar levels, which can lead to a need for adjustments in insulin dosage for patients with diabetes.
Lifestyle Modifications and Hypoglycemia Prevention
Maintaining a healthy lifestyle is crucial in preventing hypoglycemia. Consider a patient who frequently skips meals and engages in intense exercise without adjusting their insulin regimen. This inconsistent approach to nutrition and exercise, combined with the medication’s effect, can lead to fluctuations in blood sugar, potentially resulting in hypoglycemia. By consistently following a balanced diet, managing exercise routines, and closely monitoring blood glucose levels, this patient could significantly reduce their risk of hypoglycemic episodes.
Dietary Patterns and Hypoglycemia Risk
A diet high in refined carbohydrates and low in fiber can significantly increase the risk of hypoglycemia. A person consuming a diet primarily composed of sugary drinks, processed foods, and white bread may experience rapid spikes and subsequent drops in blood sugar. The lack of fiber in the diet hinders the slow release of glucose into the bloodstream, leading to a quick surge followed by a sudden crash.
This erratic blood sugar pattern can trigger hypoglycemic episodes, making it crucial to consume a balanced diet with plenty of whole grains, fruits, and vegetables.
Hypoglycemia Episode Symptoms and Treatment
Recognizing the symptoms of hypoglycemia is essential for timely treatment. Common symptoms include shakiness, sweating, rapid heartbeat, dizziness, confusion, difficulty concentrating, and blurred vision. If these symptoms occur, the immediate treatment involves consuming fast-acting carbohydrates such as glucose tablets, fruit juice, or a sugary drink. Monitoring blood sugar levels regularly is crucial to ensure that the treatment is effective and that hypoglycemia doesn’t recur.
Case Study: Patient with Multiple Risk Factors
A 50-year-old female patient with type 2 diabetes, a history of heart failure, and a recent diagnosis of depression exhibits several risk factors for hypoglycemia. She is prescribed insulin to manage her blood sugar levels, beta-blockers for her heart condition, and antidepressants for her depression. She frequently skips meals due to her busy schedule and sometimes exercises intensely without adjusting her insulin intake.
This combination of factors increases her susceptibility to hypoglycemia. Close monitoring of blood glucose levels, dietary adjustments, and consistent communication with her healthcare team are vital for managing this complex case and preventing severe hypoglycemic events.
Closing Summary: Hypoglycemia Causes Risk Factors
In conclusion, hypoglycemia, characterized by low blood sugar, stems from a multitude of interconnected factors. From underlying medical conditions to lifestyle choices, a range of risk factors contribute to the development of this condition. Understanding these causes and mitigating risk factors through proactive measures is essential for preventing serious complications. Early intervention and management are crucial in preventing the long-term effects of hypoglycemia.
By recognizing the intricate interplay of factors, individuals can better manage their risk and maintain optimal health.




