Fluid behind the retina: a common yet often misunderstood condition. This in-depth exploration delves into the various types of fluid buildup, their causes, symptoms, and treatment options. We’ll examine the normal fluid dynamics of the eye, comparing and contrasting them with abnormal accumulations behind the retina. Understanding this intricate process is crucial for comprehending the potential impact on vision and overall eye health.
From defining the different types of fluids that can accumulate behind the retina to discussing their origins, this article provides a thorough overview. We’ll cover the common causes and risk factors, explore the diverse symptoms and diagnostic methods, and analyze the available treatment options. The visual impact and long-term prognosis of this condition will also be addressed.
Fluid Behind the Retina
Fluid accumulation behind the retina, a condition often associated with various eye diseases, is a significant concern for ophthalmologists. Understanding the types of fluids, their normal function, and abnormal accumulations is crucial for accurate diagnosis and effective treatment. This detailed look at the topic will clarify the different types of fluids found behind the retina and their associated conditions.
Definition and Types of Fluid
Fluid behind the retina refers to the abnormal accumulation of liquid or other substances in the space between the retina and the underlying retinal pigment epithelium (RPE). This accumulation can stem from various causes, each with distinct characteristics. The normal fluid dynamics of the eye are critical to maintaining a healthy retina. The retina, a light-sensitive tissue, requires a precisely regulated fluid environment to function optimally.
Normal Fluid Dynamics of the Eye
The eye maintains a delicate balance of fluids, primarily aqueous humor and vitreous humor. Aqueous humor, produced by the ciliary body, nourishes the front of the eye and helps maintain intraocular pressure. Vitreous humor, a transparent gel, fills the space behind the lens and supports the retina. These fluids play critical roles in maintaining the shape and structural integrity of the eye, providing nutrition to ocular tissues, and ensuring proper retinal function.
Disruptions in this balance can lead to abnormal fluid accumulations.
Types of Fluid Accumulation
Fluid accumulation behind the retina can manifest in several forms, each with varying characteristics and potential implications. These accumulations often reflect underlying pathologies, and their presence indicates a need for careful ophthalmological evaluation.
Comparison of Fluid Accumulations
Normal fluid dynamics in the eye involve a constant exchange of fluids, maintaining a precise balance crucial for retinal health. However, pathological conditions can disrupt this balance, leading to fluid buildup. For instance, in macular edema, fluid accumulates in the macula, the central part of the retina responsible for sharp vision. This fluid accumulation can impair vision.
Fluid buildup behind the retina can be a tricky issue, sometimes mimicking symptoms of other conditions. Understanding different types of inflammatory diseases, like types of rheumatoid arthritis , is important for proper diagnosis. This is because similar inflammation can sometimes cause eye issues, though it’s crucial to remember that fluid behind the retina isn’t directly linked to these conditions, but can potentially be a symptom of an underlying problem.
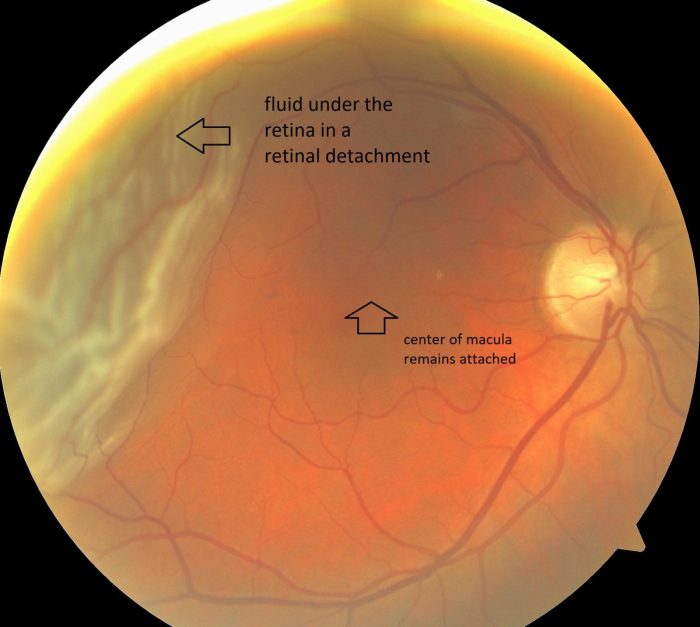
Similarly, in retinal detachment, fluid can accumulate between the retina and the retinal pigment epithelium, causing the retina to detach from its supporting structures. These conditions represent significant departures from the normal fluid dynamics and necessitate prompt medical intervention.
Summary Table of Fluid Types
| Fluid Type | Description | Causes | Symptoms |
|---|---|---|---|
| Aqueous Humor | Clear, watery fluid in the anterior chamber | Increased production, blocked drainage | Eye pain, blurred vision, redness |
| Vitreous Humor | Transparent gel in the vitreous cavity | Vitreous hemorrhage, posterior vitreous detachment | Floaters, flashes of light, vision changes |
| Subretinal Fluid | Fluid beneath the retina | Retinal detachment, macular edema, choroidal neovascularization | Blurred vision, distortion, floaters, reduced visual acuity |
| Intraretinal Fluid | Fluid within the retinal layers | Macular edema, diabetic retinopathy, inflammatory conditions | Blurred vision, distortion, reduced visual acuity |
Causes and Risk Factors
Fluid buildup behind the retina, a condition often associated with various eye diseases, can significantly impair vision. Understanding the underlying causes and risk factors is crucial for early detection and appropriate management. This knowledge allows for proactive measures to minimize the risk of vision loss.The accumulation of fluid behind the retina can stem from a multitude of systemic and ocular conditions.
The precise mechanisms involved in fluid leakage vary depending on the specific cause, but often involve disruptions in the delicate balance of vascular pressure and fluid drainage within the eye. This can lead to edema and subsequent vision impairment.
Common Causes of Fluid Buildup
Several conditions can lead to the accumulation of fluid behind the retina. These include age-related macular degeneration (AMD), diabetic retinopathy, and retinal vein occlusion. Understanding the underlying mechanisms of these conditions is essential to comprehend the fluid leakage process.
Mechanisms of Fluid Accumulation
The precise mechanisms behind fluid accumulation vary based on the underlying cause. In age-related macular degeneration, the breakdown of the macula, the central part of the retina responsible for sharp vision, can disrupt the normal functioning of the blood vessels, leading to fluid leakage. Diabetic retinopathy involves damage to the blood vessels in the retina due to high blood sugar levels.
This damage can cause weakened vessel walls and subsequent fluid leakage. Retinal vein occlusion involves blockage of blood flow in retinal veins, leading to increased pressure and fluid leakage into the surrounding tissues.
Risk Factors for Fluid Buildup
Certain factors increase the susceptibility to fluid buildup behind the retina. These factors often overlap with the causes themselves, highlighting the interconnectedness of various health factors.
- Age: The risk of age-related macular degeneration, a significant contributor to fluid buildup, increases with age. Studies have shown a correlation between advancing age and the prevalence of this condition.
- Diabetes: Individuals with diabetes are at a heightened risk of developing diabetic retinopathy, a leading cause of vision loss. Uncontrolled blood sugar levels contribute to the damage of blood vessels in the eye, increasing the likelihood of fluid leakage.
- High Blood Pressure: Elevated blood pressure can strain blood vessels, increasing the risk of leakage and potentially leading to retinal vein occlusion. This is a serious risk factor that needs to be actively managed.
- Smoking: Smoking significantly increases the risk of various eye diseases, including age-related macular degeneration. The harmful effects of smoking on the vascular system contribute to the likelihood of fluid accumulation.
- Family History: A family history of eye diseases like age-related macular degeneration or glaucoma can increase an individual’s susceptibility to fluid buildup behind the retina.
Table of Diseases and Conditions
This table summarizes various conditions that can cause fluid behind the retina, highlighting the mechanisms and risk factors associated with each.
| Condition | Mechanism | Risk Factors |
|---|---|---|
| Age-related Macular Degeneration (AMD) | Breakdown of the macula, disrupting blood vessel function, leading to fluid leakage. | Age, smoking, genetics, high cholesterol, obesity. |
| Diabetic Retinopathy | Damage to blood vessels in the retina due to high blood sugar levels, leading to weakened vessel walls and fluid leakage. | Diabetes, high blood pressure, smoking, obesity, genetics. |
| Retinal Vein Occlusion | Blockage of blood flow in retinal veins, causing increased pressure and fluid leakage into surrounding tissues. | High blood pressure, high cholesterol, smoking, age, cardiovascular disease. |
| Glaucoma | Increased intraocular pressure damaging the optic nerve, leading to potential fluid leakage in the retina. | Age, family history, high myopia, African descent. |
| Central Serous Chorioretinopathy (CSCR) | Fluid accumulation beneath the retinal pigment epithelium, typically caused by an imbalance of the choroidal circulation. | Stress, pregnancy, medications. |
Symptoms and Diagnosis: Fluid Behind The Retina
Understanding the symptoms of fluid buildup behind the retina is crucial for timely diagnosis and treatment. This fluid accumulation, often a consequence of various underlying conditions, can manifest in a range of visual disturbances. Accurate identification of these symptoms and subsequent diagnostic procedures are essential steps in determining the appropriate course of action.
Common Symptoms
Fluid accumulation behind the retina frequently presents with noticeable visual changes. These changes can range from subtle to severe, depending on the extent of the fluid buildup and the underlying cause. Common symptoms include blurry vision, distortion of images, and the perception of floaters. These floaters can appear as specks, strands, or cobwebs that drift across the field of vision.
Diminished vision, in particular, is a significant concern, potentially indicative of significant retinal detachment.
Variability in Symptoms
The specific symptoms of fluid buildup behind the retina can differ based on the underlying cause. For instance, in cases of macular edema, a common symptom is the blurring of central vision, impacting the ability to read or perform tasks requiring detailed focus. In contrast, retinal detachment often manifests with a sudden onset of floaters, flashes of light, and a sensation of a curtain descending over the vision.
The severity and type of symptom provide valuable clues for the ophthalmologist in pinpointing the cause.
Diagnostic Methods
Several diagnostic methods are employed to identify fluid buildup behind the retina. A comprehensive eye examination is fundamental. This typically involves visual acuity testing to assess the clarity of vision, ophthalmoscopy to examine the retina directly, and dilated fundus photography to capture detailed images of the retina’s structure. These procedures are critical in determining the presence and extent of fluid accumulation.
Diagnostic Procedure
A step-by-step procedure for diagnosing fluid behind the retina often involves:
- Initial Evaluation: A thorough review of the patient’s medical history, including any pre-existing conditions, medications, and recent eye injuries, is crucial. This step helps establish a baseline understanding of the patient’s condition and potential contributing factors.
- Visual Acuity Testing: Precise measurements of the patient’s visual sharpness are recorded to evaluate the clarity and extent of vision impairment.
- Ophthalmoscopy: A specialized instrument allows the ophthalmologist to directly view the retina, enabling visualization of any fluid buildup, swelling, or detachment.
- Dilated Fundus Photography: High-resolution images of the retina are captured to document the condition and aid in comparison with future examinations or for potential follow-up.
- Additional Tests: Depending on the suspected cause, additional tests such as optical coherence tomography (OCT) might be necessary to create detailed cross-sectional images of the retina and measure the thickness of retinal layers.
Symptom Significance Table
| Symptom | Description | Possible Cause |
|---|---|---|
| Blurred vision | Loss of clarity in vision | Macular edema, retinal detachment, vitreous hemorrhage |
| Floaters | Small, moving specks or strands in the visual field | Retinal detachment, vitreous inflammation, posterior vitreous detachment |
| Flashes of light | Sudden, brief bursts of light | Retinal detachment, vitreous inflammation |
| Diminished vision | Significant reduction in visual clarity | Retinal detachment, macular edema, glaucoma |
| Distorted vision | Images appear warped or misshapen | Macular edema, retinal detachment, high myopia |
Treatment and Management
Managing fluid buildup behind the retina requires a multifaceted approach tailored to the underlying cause and the severity of the condition. Treatment options range from observation and supportive care to more invasive procedures, all aimed at reducing the fluid, preventing further damage, and restoring vision. The effectiveness and potential complications of each treatment will vary depending on individual circumstances.
Treatment Options
Various treatment strategies are available for managing fluid accumulation behind the retina, each with its own rationale and potential outcomes. These options often involve a combination of approaches depending on the specific situation.
Surgical Interventions
Surgical interventions, including vitrectomy, are sometimes necessary for cases where fluid buildup significantly compromises vision or is unresponsive to other treatments. Vitrectomy involves removing the vitreous gel, the transparent jelly-like substance that fills the eye. This procedure allows access to the retina to remove fluid and scar tissue, potentially restoring or improving vision. The rationale for vitrectomy is to remove the causative agent and allow for better visualization and treatment of the underlying retinal problem.
Complications can include retinal detachment, infection, and bleeding. The effectiveness of vitrectomy depends on the cause and severity of the fluid buildup and the individual’s overall health.
Ever wondered about fluid buildup behind the retina? It’s a tricky issue, and honestly, I’ve been researching a lot about it lately. It can be a side effect of various things, and sometimes it’s linked to changes in the body after a major surgery like a hysterectomy. Understanding how your body changes after this procedure is crucial, and resources like your body after hysterectomy offer valuable insights.
Learning more about the potential impacts on your overall health can help you understand the fluid buildup issue better. So, next time you consider this, think about the bigger picture!
Pharmacological Treatments
Pharmacological treatments, such as anti-VEGF injections, are often used to reduce the production of vascular endothelial growth factor (VEGF), a protein that contributes to fluid leakage. These injections are administered directly into the eye. The rationale behind these treatments is to inhibit the growth of abnormal blood vessels that contribute to fluid leakage, thereby reducing swelling and inflammation. Potential side effects include eye pain, inflammation, and infection at the injection site.
The effectiveness of anti-VEGF injections varies depending on the underlying cause and the patient’s response.
Laser Treatments
Laser treatments, such as laser photocoagulation, are employed to seal leaky blood vessels in the retina. The rationale for this approach is to prevent further fluid leakage and potential retinal damage. The procedure involves precisely targeting and destroying small areas of the retina. Potential complications include damage to healthy retinal tissue and scarring. The effectiveness of laser treatments is highly dependent on the location and extent of the retinal leakage.
Table of Treatment Modalities
| Treatment | Description | Effectiveness | Potential Side Effects |
|---|---|---|---|
| Vitrectomy | Surgical removal of the vitreous gel to access and treat the retina. | Potentially effective in severe cases, but carries risk. | Retinal detachment, infection, bleeding, and possible loss of vision. |
| Anti-VEGF Injections | Injections of medications that inhibit VEGF production to reduce fluid leakage. | Often effective for macular edema and other conditions. | Eye pain, inflammation, infection, and rare cases of retinal detachment. |
| Laser Photocoagulation | Laser treatment to seal leaky blood vessels in the retina. | Can be effective for controlling leakage, but not always a first-line treatment. | Damage to healthy retinal tissue, scarring, and potential loss of vision. |
| Observation and Supportive Care | Close monitoring without immediate intervention for less severe cases. | Effective for cases with slow progression. | Potential for vision loss if condition worsens. |
Visual Impact and Prognosis
Fluid buildup behind the retina can significantly impair vision, ranging from mild blurring to complete loss of sight. The severity of the vision loss is directly tied to the amount of fluid accumulated and the specific location of the buildup. Understanding the potential impact on vision is crucial for effective management and prognosis.
Impact on Vision
Fluid accumulation can distort the light-sensitive cells in the retina, impairing the eye’s ability to focus and transmit clear images to the brain. This leads to blurred vision, reduced visual acuity, and potentially, distorted or double vision. The precise nature of the visual disturbance depends on the location and extent of the fluid. For instance, fluid accumulating near the macula, the central part of the retina responsible for sharp central vision, will likely have a more significant impact on detail and clarity compared to fluid in the periphery.
Correlation with Severity
The severity of visual impairment is directly correlated with the amount of fluid behind the retina. Mild fluid buildup may cause only slight blurring or haziness, while more substantial accumulation can lead to significant distortion or loss of vision. Factors such as the rate of fluid accumulation, the underlying cause, and the individual’s overall eye health also play a role in the extent of visual impact.
Prognosis, Fluid behind the retina
The prognosis for patients with fluid behind the retina varies greatly depending on the underlying cause, the response to treatment, and the individual’s overall health. For conditions like macular edema secondary to diabetic retinopathy, treatment focused on managing the underlying diabetes and addressing the inflammation can often lead to some improvement in vision. However, in cases of severe fluid buildup or if the cause is not effectively managed, the prognosis may be less favorable.
Fluid buildup behind the retina can sometimes be a tricky issue to diagnose. It’s important to consider your overall physical activity and how your body responds to exertion. Understanding your rate of perceived exertion ( rate of perceived exertion ) can be a helpful tool for gauging the strain on your body. This can help in identifying potential underlying causes and monitoring the fluid levels.
Ultimately, careful monitoring of this fluid accumulation is crucial for maintaining good eye health.
The likelihood of regaining lost vision is influenced by how quickly the fluid is managed and the extent of damage to the retina. For instance, if the fluid buildup is caused by a sudden, traumatic event, the potential for recovery is often lower.
Long-Term Effects
Long-term effects of fluid buildup behind the retina can range from minor, persistent vision changes to significant and irreversible vision loss. If the fluid accumulation is not properly addressed, it can lead to permanent damage to the retina, affecting the patient’s ability to perform everyday tasks that require clear vision.
Stages of Fluid Accumulation and Visual Impact
| Stage | Fluid Amount | Visual Acuity | Prognosis |
|---|---|---|---|
| Mild | Small accumulation | Slight blurring, reduced clarity | Good, often reversible with treatment |
| Moderate | Moderate accumulation | Significant blurring, distortion | Moderate, potential for partial vision recovery with treatment |
| Severe | Large accumulation | Marked distortion, significant loss of central vision | Variable, depends on the underlying cause and treatment response. Potential for irreversible vision loss. |
Note: Visual acuity is measured in decimal values (e.g., 20/20, 20/40, etc.). This table is a general guide and individual cases may vary.
Illustrations and Examples
Understanding fluid buildup behind the retina requires visualizing both a healthy retina and the various stages of fluid accumulation. This section provides detailed descriptions of retinal structures, fluid buildup appearances, imaging techniques, and the layers affected. This will aid in comprehending the complexities of this condition.
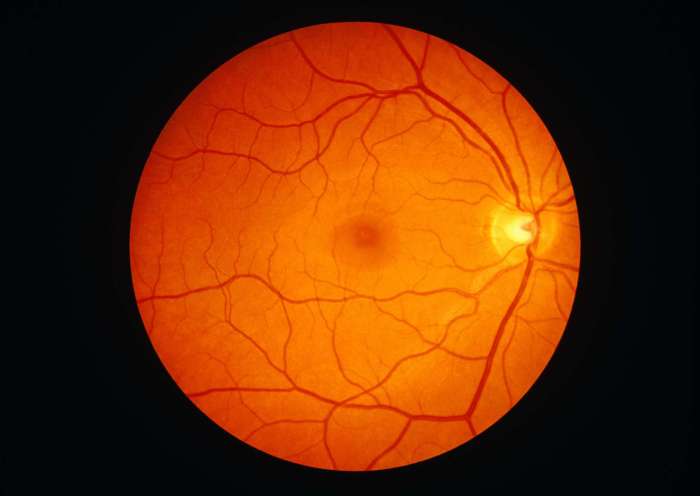
Healthy Retinal Structure
The retina, a thin layer of tissue lining the back of the eye, is a complex structure crucial for vision. It comprises several distinct layers, each playing a specific role in converting light into signals the brain interprets as images. A healthy retina maintains a precise arrangement of these layers. The photoreceptor cells (rods and cones), responsible for detecting light, are situated at the back of the retina.
Behind them lies the pigmented epithelium, a layer that absorbs stray light and nourishes the photoreceptors. Further inwards, there are various neuronal layers, including bipolar cells and ganglion cells, which transmit signals to the optic nerve. The precise arrangement and integrity of these layers are vital for optimal vision.
Fluid Buildup Appearance
Fluid accumulation behind the retina can manifest in various ways, progressing through different stages. Initially, the fluid may appear as subtle swelling or clouding in specific retinal areas. As the condition progresses, the fluid buildup may become more pronounced, potentially leading to a larger area of swelling or even a cystic appearance, resembling fluid-filled sacs within the retina.
Severe cases may show a diffuse and extensive fluid collection that significantly distorts the normal retinal architecture. Different stages involve varying degrees of fluid density and distribution across the retina.
Imaging Techniques
Several advanced imaging techniques are employed to visualize fluid buildup behind the retina. Optical coherence tomography (OCT) is a non-invasive technique that provides detailed cross-sectional images of the retina. OCT scans can clearly depict the presence and extent of fluid within the retinal layers. OCT angiography (OCT-A) enhances these capabilities by visualizing the retinal blood vessels, aiding in differentiating fluid from other retinal abnormalities.
Fluorescein angiography (FA) involves injecting a fluorescent dye into the bloodstream. As the dye circulates, it highlights the retinal blood vessels, enabling visualization of any leakage or abnormalities in the blood vessels that may correlate with fluid accumulation. These techniques provide valuable insights into the nature and severity of the fluid buildup.
Retinal Layers Involved
Fluid buildup behind the retina can affect several retinal layers. The precise location of the fluid accumulation often correlates with the underlying cause and the specific retinal layers involved. Fluid can accumulate within the inner retinal layers, disrupting the normal transmission of signals from photoreceptors to the optic nerve. Alternatively, fluid may accumulate in the subretinal space, the area between the retinal pigment epithelium and the photoreceptor layer.
Understanding the affected layers is crucial for accurate diagnosis and appropriate treatment strategies.
Final Conclusion
In conclusion, fluid buildup behind the retina is a multifaceted issue requiring a nuanced understanding of its causes, symptoms, and treatments. This guide has provided a comprehensive overview of the topic, from the definition and underlying mechanisms to the potential impact on vision and the available management strategies. We hope this article has shed light on this often-overlooked condition and empowered readers with a greater understanding of its complexities.




