Uterus location function female anatomy explores the fascinating position and role of the uterus within the female body. From its placement in the pelvis to its crucial functions in menstruation, fertilization, and pregnancy, this comprehensive guide delves into the intricate details of this vital organ.
We’ll examine the uterus’s relationship to surrounding organs like the bladder and rectum, and explore its structure, from the body and fundus to the cervix and endometrium. Furthermore, we’ll cover the various stages of the menstrual cycle and the impact of pregnancy on uterine function. We’ll also touch on common conditions and diagnostic methods to ensure a complete understanding of this essential part of female anatomy.
Uterine Location
The uterus, a crucial part of the female reproductive system, sits deep within the female pelvis, nestled between other vital organs. Understanding its precise anatomical position is vital for comprehending its function and potential health concerns. This section delves into the uterus’s location, its relationships with surrounding structures, and how this positioning varies throughout a woman’s reproductive life.The uterus is a hollow, pear-shaped organ positioned centrally within the female pelvis, tilted slightly forward towards the pubic bone.
Its position and orientation are influenced by the surrounding structures and, importantly, by the stage of the menstrual cycle or pregnancy.
Anatomical Position in the Pelvis
The uterus occupies a central location within the female pelvis, anterior to the rectum and posterior to the bladder. Its superior portion, or fundus, is above the openings of the fallopian tubes. This central positioning allows it to effectively receive and support a fertilized ovum during pregnancy. The cervix, the lower portion of the uterus, extends into the vagina.
This anatomical arrangement facilitates the passage of the fetus during childbirth.
Relationship to Pelvic Organs
The uterus interacts with and is positioned relative to several other pelvic organs. The bladder lies anteriorly, meaning in front of the uterus. The rectum is situated posteriorly, behind the uterus. The ovaries, the female reproductive glands, are situated laterally, on either side of the uterus, connected by fallopian tubes. These relationships are crucial for maintaining proper pelvic function and preventing potential interference between organs.
Understanding the relative positions of these organs can aid in diagnosis and treatment of pelvic pain or other issues.
Uterine Position in Different Reproductive Stages
| Reproductive Stage | Uterine Position (Anterior/Posterior Tilt) | Comments ||—|—|—|| Menstrual | Slightly anteverted (tilted forward) | Typically, the uterus is in a relatively stable position during the menstrual phase. || Ovulatory | Slightly anteverted (tilted forward) | No significant change in position compared to the menstrual phase. || Pregnancy (Early) | Slightly anteverted (tilted forward) | Early pregnancy typically does not result in a substantial shift in uterine position.
|| Pregnancy (Mid) | Anteverted, gradually becoming more fixed | The uterus enlarges, and its position is more fixed as the pregnancy progresses. The growing uterus might push against the bladder, causing more frequent urination. || Pregnancy (Late) | Anteverted, more elevated | As the uterus grows larger, it ascends into the abdominal cavity, continuing to be anteverted.
Understanding the uterus’s location and function within female anatomy is crucial. It’s a fascinating organ, nestled in the pelvis, supporting the development of a fetus. While we’re on the topic of female health, did you know that some people believe raw milk has various potential benefits for overall well-being? Exploring the potential advantages of raw milk could be interesting for those considering different dietary approaches.
Ultimately, consulting with a healthcare professional about the uterus and its role in women’s health is always recommended. benefits of raw milk This knowledge is vital for comprehending the complexities of the female reproductive system.
|| Postpartum | Anteverted, gradually returning to normal position | After childbirth, the uterus contracts and returns to its pre-pregnancy position. |The table above highlights the general position of the uterus in different reproductive stages. It’s important to remember that individual variations exist. This table provides a generalized view of how the uterus’s position might change. For instance, a fibroid or other abnormalities can affect the uterus’s positioning.
Uterine Function
The uterus, a crucial organ in the female reproductive system, plays a multifaceted role in supporting the continuation of life. Beyond its anatomical location, its physiological functions are vital for menstruation, potential fertilization, and pregnancy. Understanding these functions provides insight into the intricate processes that govern a woman’s reproductive health.The uterus’s primary role is to nurture and support a developing embryo during pregnancy.
This includes providing a safe and nourishing environment for the fertilized egg to implant, grow, and develop into a fetus. The complex interactions between the uterine lining, hormones, and the developing embryo are central to successful gestation. This dynamic interplay shapes the physiological changes experienced by women throughout their reproductive years.
Key Functions in Reproduction
The uterus is more than just a container; it’s a dynamic organ that actively participates in the complex process of reproduction. Its key functions include providing a site for implantation, nourishing the developing embryo, and contracting to expel the fetus during childbirth.
Role in Menstruation
Menstruation is a regular shedding of the uterine lining, or endometrium, when pregnancy does not occur. The endometrium thickens in preparation for potential implantation. If fertilization doesn’t occur, the thickened lining is shed, resulting in menstruation. This process is controlled by fluctuating hormone levels, primarily estrogen and progesterone.
Role in Fertilization
Fertilization, the fusion of sperm and egg, marks the beginning of potential pregnancy. The uterus plays a vital role in ensuring that a fertilized egg can successfully implant in the endometrium. The uterine environment is carefully orchestrated to create an optimal environment for this delicate process.
Role in Pregnancy
If fertilization occurs, the uterus undergoes significant changes to support the developing embryo. The uterine wall thickens and develops specialized structures to provide nourishment and protection to the growing fetus. This process, which continues for approximately nine months, involves a complex interplay of hormonal and cellular processes.
Stages of Uterine Development and Growth
The uterus’s size and structure change throughout a woman’s life, adapting to the different phases of her reproductive cycle. From puberty to menopause, the uterus’s function and structure are closely tied to the hormonal fluctuations that govern a woman’s reproductive capabilities. These changes can be categorized into several phases, each characterized by specific physiological and structural adaptations.
- Puberty: The uterus begins to mature under the influence of hormones, increasing in size and developing the capacity to support a potential pregnancy.
- Reproductive Years: The uterus cycles through the menstrual phases, thickening and shedding its lining in preparation for pregnancy. The uterus’s size and structure remain relatively consistent during these years, ready to support the development of a fetus.
- Menopause: As hormone levels decline, the uterus gradually undergoes structural changes. These changes typically result in a decrease in the size and thickness of the uterus.
Uterine Lining (Endometrium) and Pregnancy Preparation
The endometrium, the inner lining of the uterus, plays a critical role in preparing for potential pregnancy. Its cyclical changes are precisely regulated by hormones to support the implantation and development of a fertilized egg. The endometrium’s complex structure and function are vital for successful reproduction.The endometrium’s thickness and vascularity change throughout the menstrual cycle, preparing for potential implantation.
This dynamic process is regulated by a complex interplay of hormones, including estrogen and progesterone. The endometrial lining is primed to accept a fertilized egg, providing a nourishing environment for its early development.
Menstrual Cycle and Uterine Changes
The menstrual cycle is a recurring cycle of hormonal changes that affect the uterus. The following table illustrates the key stages and the corresponding uterine changes:
| Stage of Menstrual Cycle | Uterine Changes |
|---|---|
| Menstruation | Shedding of the thickened endometrial lining |
| Proliferative Phase | Endometrium thickens and develops under the influence of estrogen |
| Secretory Phase | Endometrium further thickens, preparing for implantation |
Female Anatomy
The female reproductive system is a complex network of organs, each playing a crucial role in the overall function. Understanding the intricate connections between these structures is vital for comprehending the delicate balance of the system. This exploration delves into the key anatomical structures associated with the uterus, highlighting their roles and connections to maintain reproductive health.
Related Structures of the Uterus
The uterus isn’t an isolated organ; it’s intricately connected to other structures, each contributing to the reproductive process. These connections facilitate the passage of eggs, sperm, and the development of a fetus.
- Fallopian Tubes: The fallopian tubes, also known as oviducts, act as conduits connecting the ovaries to the uterus. These tubes are crucial for transporting the ovum from the ovary to the uterus. Fertilization typically occurs within the fallopian tubes. The fimbriae, finger-like projections at the end of the fallopian tubes, play a critical role in capturing the released ovum.
The muscular contractions of the fallopian tubes aid in the movement of the ovum.
- Cervix: The cervix is the lower portion of the uterus, connecting it to the vagina. It acts as a gatekeeper, regulating the passage of sperm and menstrual flow. The cervix’s unique muscular and connective tissue structure facilitates its function in maintaining the integrity of the reproductive tract. During pregnancy, the cervix thickens and becomes more resilient to support the developing fetus.
- Ovaries: The ovaries are responsible for producing eggs (ova) and the hormones estrogen and progesterone. These hormones regulate the menstrual cycle and are essential for maintaining a healthy reproductive system. The ovaries are located on either side of the uterus, linked to the fallopian tubes through the ovarian ligaments. The ovaries’ cyclical activity directly influences the uterine lining’s preparation for potential pregnancy.
- Vagina: The vagina is the muscular canal that extends from the cervix to the external genitalia. It serves as the birth canal and is the passageway for menstrual flow. The vagina’s elasticity and flexibility are crucial for both sexual intercourse and childbirth. It’s also a conduit for the introduction of sperm into the reproductive tract.
Comparison of Reproductive Organs
Comparing the uterus to other reproductive organs reveals unique structural and functional adaptations. The uterus’s thick muscular wall is essential for supporting pregnancy and facilitating labor. The ovaries, while integral to the reproductive cycle, primarily focus on hormone production and egg development. The fallopian tubes’ primary role is transportation, while the cervix maintains the structural integrity of the uterus.
| Organ | Primary Function | Connection to Uterus |
|---|---|---|
| Uterus | Site of fetal development | Connected to fallopian tubes and cervix |
| Fallopian Tubes | Transport ovum | Connect ovaries to uterus |
| Ovaries | Produce eggs and hormones | Connected to fallopian tubes, influence uterine lining |
| Cervix | Regulates passage of sperm and menstrual flow | Connects uterus to vagina |
| Vagina | Birth canal, passageway for menstrual flow | Receives cervix |
Uterine Support Ligaments
Several ligaments play crucial roles in supporting the uterus’s position within the pelvis. Their structural integrity ensures proper positioning for optimal function.
| Ligament | Function |
|---|---|
| Broad Ligaments | Support the uterus, ovaries, and fallopian tubes, holding them in place within the pelvis. |
| Round Ligaments | Help maintain the forward tilt of the uterus and prevent excessive movement. |
| Cardinal (Mackenrodt) Ligaments | Provide significant support to the cervix and upper vagina, preventing prolapse. |
| Uterosacral Ligaments | Stabilize the uterus by connecting it to the sacrum, contributing to its posterior support. |
Uterine Structure
The uterus, a vital organ in the female reproductive system, is a muscular, pear-shaped structure that houses the developing fetus during pregnancy. Understanding its intricate structure is crucial for comprehending its function and potential issues. This section delves into the key components of the uterus, its wall layers, and the uterine cavity, providing a detailed overview of this essential organ.
Key Structural Components
The uterus is composed of several distinct parts. The body of the uterus is the major portion, tapering down to the cervix. The fundus is the rounded top portion of the uterus, located above where the fallopian tubes connect. The cervix, a narrow neck of tissue, connects the uterus to the vagina. These components work in concert to facilitate the processes of menstruation, fertilization, and pregnancy.
Layers of the Uterine Wall
The uterine wall is composed of three distinct layers, each with a specific role. The perimetrium is the outermost serous membrane that covers the uterus. The myometrium is the thick, muscular layer responsible for powerful contractions during childbirth. The endometrium is the inner lining of the uterus, undergoing cyclical changes throughout the menstrual cycle to prepare for potential implantation.
These layers work in harmony to support pregnancy and regulate the menstrual cycle.
Uterine Cavity
The uterine cavity is the hollow, interior space of the uterus. It is a dynamic environment, changing shape and size during the menstrual cycle and pregnancy. The shape of the uterine cavity is typically fusiform, with a larger superior portion and a narrowing inferior portion that leads to the cervix. This cavity allows for the development and growth of the embryo/fetus.
Dimensions of the Uterus
| Reproductive Stage | Length (cm) | Width (cm) | Thickness (cm) |
|---|---|---|---|
| Pre-menarche | 5-7 | 3-4 | 2-3 |
| Reproductive Years | 7-8 | 5-6 | 2-4 |
| Post-menopause | 5-6 | 3-4 | 1-2 |
Note: These are approximate dimensions and can vary based on individual factors.
The uterus, a crucial part of the female reproductive system, sits in the pelvis, supporting the development of a fertilized egg. Understanding its location and function is fundamental to female anatomy. However, sometimes, a disease like breast cancer can spread to other parts of the body, such as the bones, lungs, or liver, as detailed in this resource on how breast cancer spreads.
Ultimately, a healthy uterus, positioned correctly, is vital for a woman’s overall well-being.
Role of Muscle Tissue in Childbirth
The myometrium, the thick muscular layer of the uterus, plays a critical role during childbirth. Powerful rhythmic contractions of the myometrium are essential for pushing the baby out of the uterus and through the birth canal. The strength and coordination of these contractions are crucial for a successful vaginal delivery. The intense force of these contractions, regulated by hormones, are vital for expulsion of the fetus.
Clinical Considerations
The female reproductive system, while remarkably resilient, is susceptible to a range of conditions that can affect uterine health. Understanding these conditions, their diagnosis, and treatment options is crucial for maintaining optimal well-being. This section will delve into common uterine issues, highlighting the impact of pregnancy on the uterus and the diagnostic and treatment approaches used by healthcare professionals.Common conditions affecting the uterine structure often manifest with a variety of symptoms, ranging from mild discomfort to severe pain.
The uterus, a crucial part of the female reproductive system, sits in the pelvis, supporting the developing fetus during pregnancy. Understanding its function is key to comprehending female anatomy, but it’s important to remember that certain respiratory conditions, like lower respiratory infections, can impact overall health, even affecting the body’s ability to function properly. For more information on what a lower respiratory infection is, check out this helpful resource: what is a lower respiratory infection.
Ultimately, the complex interplay of various body systems highlights the interconnectedness of health, and proper knowledge of female anatomy remains vital for well-being.
Accurate diagnosis and timely intervention are essential for effective management. This section provides an overview of these conditions and the methods employed to identify and treat them.
Common Uterine Conditions
A range of conditions can impact the uterus, affecting its structure and function. Uterine fibroids, endometriosis, and uterine prolapse are among the most prevalent. These conditions may lead to a variety of symptoms and necessitate careful evaluation and management.
- Uterine Fibroids: These benign tumors, composed of smooth muscle and connective tissue, can develop within the uterine wall. They are often asymptomatic, but larger fibroids can cause heavy menstrual bleeding, pelvic pain, pressure, and sometimes infertility. Fibroids can vary greatly in size and location, and their impact on the uterus can differ significantly.
- Endometriosis: This condition involves the growth of endometrial tissue outside the uterus, often affecting the ovaries, fallopian tubes, and surrounding tissues. Symptoms may include pelvic pain, heavy bleeding, painful periods, and discomfort during sexual intercourse. The presence of endometrial tissue outside the uterus can lead to inflammation and scarring, potentially affecting fertility.
- Uterine Prolapse: This occurs when the uterus descends from its normal position in the pelvis. Several factors, including childbirth, hormonal changes, and weakened pelvic floor muscles, can contribute to this condition. Symptoms may include pelvic pressure, discomfort, and a feeling of heaviness in the pelvis. Uterine prolapse can range in severity, with mild cases potentially manageable with supportive measures, while more severe cases may necessitate surgical intervention.
Diagnostic Methods
Accurate diagnosis is crucial for effective treatment planning. Various diagnostic methods are employed to assess uterine health, including imaging and invasive procedures.
- Ultrasound: This non-invasive imaging technique uses sound waves to create images of the uterus and surrounding structures. Transvaginal ultrasounds, performed with a probe inserted into the vagina, provide detailed images of the uterine lining and surrounding tissues, aiding in the detection of fibroids, cysts, and other abnormalities. Abdominal ultrasounds, performed with a probe placed on the abdomen, provide a broader view of the pelvic organs.
- Hysteroscopy: This procedure involves inserting a thin, flexible tube with a camera (hysteroscope) into the uterus through the cervix. This allows direct visualization of the uterine cavity, enabling the detection of polyps, fibroids, and other abnormalities. It can also be used for certain surgical procedures.
- Biopsy: A tissue sample is taken from the uterus for microscopic examination. This can help diagnose various conditions, including cancer and other pathologies. The biopsy procedure is typically performed under guidance from imaging techniques, such as ultrasound or hysteroscopy.
Treatment Options
Treatment approaches for uterine conditions vary depending on the specific condition, its severity, and the patient’s individual circumstances.
- Medical Management: Medications, such as hormonal therapies, can be used to manage symptoms of conditions like endometriosis and uterine fibroids. Hormonal treatments may reduce the size of fibroids or regulate menstrual cycles.
- Minimally Invasive Surgery: Procedures like laparoscopy and myomectomy (surgical removal of fibroids) are often used for conditions like endometriosis, fibroids, and uterine prolapse. These procedures minimize incisions and promote faster recovery.
- Surgical Interventions: In more severe cases, such as advanced uterine prolapse, hysterectomy (surgical removal of the uterus) may be necessary.
Pregnancy and the Uterus
Pregnancy profoundly impacts the uterus. The uterus expands significantly to accommodate the growing fetus. The uterine lining thickens to support the developing embryo, and the blood supply increases to meet the needs of the growing baby. These changes are critical for a healthy pregnancy and fetal development. The increasing size and weight of the uterus can cause pressure on other organs and lead to changes in posture and balance.
Table of Uterine Conditions
| Condition | Symptoms | Potential Treatments |
|---|---|---|
| Uterine Fibroids | Heavy bleeding, pelvic pain, pressure, infertility | Hormonal therapy, myomectomy, hysterectomy |
| Endometriosis | Pelvic pain, heavy bleeding, painful periods, discomfort during intercourse | Hormonal therapy, laparoscopic surgery, pain management |
| Uterine Prolapse | Pelvic pressure, discomfort, heaviness, a feeling of descent | Pessary, pelvic floor exercises, surgery |
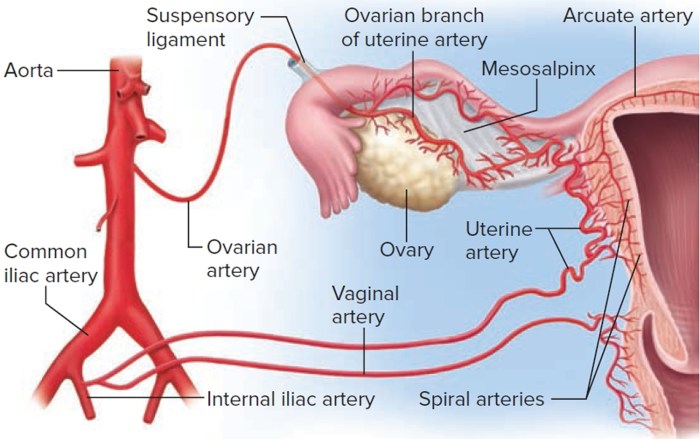
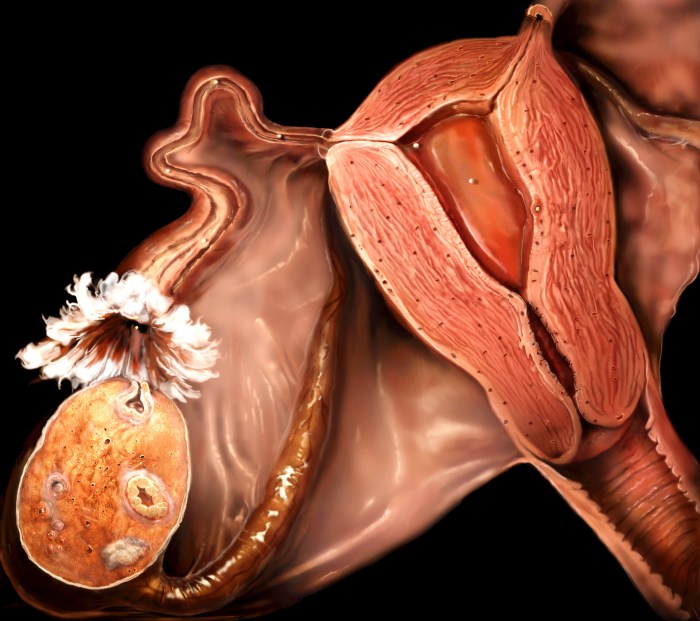
Illustrations and Visualizations: Uterus Location Function Female Anatomy
Visual aids play a crucial role in understanding complex biological systems like the female reproductive system. Illustrations and models allow us to visualize the intricate relationships between different organs and structures, enhancing our comprehension of their functions and interactions. These tools aid in education, diagnosis, and research, facilitating a deeper understanding of the female anatomy and physiology.
3D Model of the Female Pelvis
A detailed 3D model of the female pelvis provides a comprehensive view of the pelvic organs, including the uterus. The model should showcase the uterus’s position within the pelvis, nestled between the bladder and the rectum. It should highlight the uterus’s anterior and posterior positions in relation to other pelvic structures. The model should clearly delineate the uterine fundus, body, and cervix, and should indicate the direction of the fallopian tubes and their connection to the ovaries.
The model should also illustrate the ligaments that support the uterus and the surrounding tissues.
Menstrual Cycle and Uterine Lining Changes, Uterus location function female anatomy
An illustration depicting the stages of the menstrual cycle should clearly show the corresponding changes in the uterine lining. The illustration should depict the proliferative phase, where the uterine lining thickens in preparation for potential pregnancy. It should also show the secretory phase, characterized by the uterine lining’s further development and vascularization. Finally, the illustration should display the shedding of the uterine lining during menstruation.
This visualization should effectively communicate the cyclical nature of the uterine lining and its response to hormonal fluctuations.
Uterine Wall Layers and Their Functions
A diagram illustrating the uterine wall layers should include the endometrium, myometrium, and perimetrium. The endometrium, the innermost layer, should be highlighted as the site of implantation and the layer that undergoes significant changes during the menstrual cycle. The myometrium, the middle layer, should be presented as the muscular layer responsible for contractions during childbirth. The perimetrium, the outermost layer, should be shown as the serous membrane covering the uterus.
Each layer should be clearly labeled, and its specific function should be concisely explained.
Fertilization and Implantation
A detailed illustration depicting the process of fertilization and implantation should start with the egg being released from the ovary and transported to the fallopian tube. The illustration should then show the process of fertilization, where the sperm fuses with the egg. The illustration should then show the zygote’s journey through the fallopian tube and into the uterus.
Finally, the illustration should depict the implantation of the fertilized egg into the uterine lining, highlighting the crucial events that lead to pregnancy. The process should be presented step-by-step, with clear labels for each stage.
Uterus and Surrounding Organs
A diagram demonstrating the structure of the uterus and its connections to surrounding organs should clearly show the uterus’s relationship with the vagina, fallopian tubes, ovaries, bladder, and rectum. The diagram should illustrate the anatomical relationships, highlighting the supportive ligaments and tissues that connect the uterus to other pelvic organs. The illustration should accurately depict the relative positions of these organs and how they interact with the uterus.
Summary
In conclusion, understanding uterus location function female anatomy is crucial for appreciating the complexity and beauty of the female reproductive system. This journey through the uterus’s position, function, and associated structures highlights its vital role in a woman’s life cycle, from development to childbirth. We hope this overview provides a solid foundation for further exploration of this remarkable organ.




