Metastatic breast cancer prognosis is a crucial aspect of understanding this complex disease. This exploration delves into the factors influencing survival, treatment approaches, and prognostic models. From tumor characteristics to patient demographics and treatment responses, we’ll uncover the key elements shaping the trajectory of metastatic breast cancer.
Understanding the factors that influence prognosis is critical for both patients and healthcare professionals. This article provides a comprehensive overview of various aspects, from tumor characteristics to treatment strategies, offering insights into the complexities of this disease. The prognosis of metastatic breast cancer is not a single, fixed outcome but a dynamic interplay of multiple factors.
Introduction to Metastatic Breast Cancer Prognosis
Metastatic breast cancer, a stage where cancer cells have spread beyond the breast to other parts of the body, presents a complex and challenging situation for patients and their healthcare teams. Understanding the prognosis, or the likely outcome, is crucial for making informed decisions about treatment options and managing expectations. The prognosis is not a simple prediction, but rather an assessment based on various factors that influence the course of the disease.
It’s important to remember that prognosis is an estimate, not a guaranteed outcome, and individual experiences can vary widely.The significance of prognosis in metastatic breast cancer lies in its ability to provide a framework for personalized care. By considering factors that influence the disease’s progression, healthcare professionals can tailor treatment strategies and support plans to maximize quality of life and extend survival time.
Accurate prognosis enables patients to make informed decisions about their treatment options, understand the potential challenges ahead, and prepare themselves emotionally and practically for the journey.
Factors Influencing Metastatic Breast Cancer Prognosis
Various factors play a critical role in shaping the prognosis of metastatic breast cancer. These factors are complex and interconnected, making it challenging to predict the exact course of the disease for each individual. Understanding these factors allows for more nuanced and effective care.
Navigating the prognosis of metastatic breast cancer can feel overwhelming. While there’s no one-size-fits-all answer, understanding the factors influencing outcomes is key. For example, knowing how to perform the the ac joint compression test might seem unrelated, but a comprehensive understanding of potential physical symptoms is part of a larger picture for overall well-being, ultimately helping to improve the quality of life for those facing this challenge.
Ultimately, prognosis depends on a multitude of variables, making each individual’s journey unique.
| Factor | Description | Impact on Prognosis | Example |
|---|---|---|---|
| Tumor Characteristics | Size, grade, type (e.g., hormone receptor status, HER2 status, triple-negative) | High-grade tumors often have a poorer prognosis compared to low-grade tumors. Specific subtypes like triple-negative breast cancer tend to have an aggressive course. | A high-grade, triple-negative breast cancer that has spread to the lungs and liver might have a shorter survival time than a lower-grade, hormone receptor-positive breast cancer that has spread to bone. |
| Extent of Metastasis | The number and location of metastases. | Metastases in multiple organs, or in organs with high metabolic activity (such as the liver or brain), tend to be more aggressive and have a poorer prognosis. | Metastatic breast cancer with lung, brain, and bone involvement often has a more challenging prognosis than cancer that has only spread to the bone. |
| Patient’s Age and Overall Health | Age, comorbidities (other medical conditions), and general physical condition | Older age and pre-existing health conditions can impact a patient’s ability to tolerate aggressive treatments, potentially affecting prognosis. | A 65-year-old patient with diabetes and cardiovascular issues might have a different prognosis than a 40-year-old patient with no significant comorbidities. |
| Treatment Response | How well the patient responds to initial and subsequent treatments | A positive response to initial therapies, like chemotherapy or targeted therapy, often indicates a better prognosis. The rate of disease progression following treatment is also a key factor. | A patient who achieves a significant reduction in tumor size and a stabilization of the disease progression after chemotherapy is likely to have a better prognosis than a patient whose cancer continues to grow despite treatment. |
| Patient’s Lifestyle and Support System | Diet, exercise, stress levels, and the support of family and friends | Healthy lifestyle choices and a strong support system can positively impact a patient’s well-being and ability to cope with the disease, which can indirectly influence the prognosis. | A patient who maintains a healthy diet, exercises regularly, and has a supportive family network may experience a better quality of life and potentially a better prognosis compared to a patient who isolates themselves and avoids healthy habits. |
Prognostic Factors
Understanding the prognosis of metastatic breast cancer hinges on identifying key factors that influence survival time. These factors, ranging from tumor characteristics to patient demographics and treatment response, provide valuable insights into individual patient trajectories. Accurate assessment of these factors aids in developing personalized treatment plans and anticipating potential outcomes.
Tumor Characteristics
Tumor characteristics play a significant role in predicting the course of metastatic breast cancer. Factors like tumor size, grade, and the presence of specific genetic alterations provide critical information. High-grade tumors, characterized by aggressive cellular growth patterns, tend to have a poorer prognosis compared to low-grade tumors. Similarly, larger tumor sizes often correlate with more advanced disease and a shorter survival time.
The presence of specific genetic alterations, such as HER2 amplification or mutations in genes like PIK3CA or TP53, can significantly impact treatment options and prognosis. These genetic alterations are often assessed using molecular testing. For example, a patient with a HER2-positive tumor might benefit from targeted therapies, potentially improving survival.
Navigating the prognosis of metastatic breast cancer can be tough, but focusing on supportive care is key. While there’s no magic bullet for easing the journey, understanding how to manage potential complications like bowel blockages is important. For instance, knowing how to address a bowel blockage at home can significantly improve comfort and quality of life. Luckily, helpful resources like this guide on how to loosen a bowel blockage at home can provide practical steps.
Ultimately, staying informed and proactive is crucial for managing the challenges that come with metastatic breast cancer.
Patient Demographics
Patient demographics, including age, ethnicity, and socioeconomic status, can also influence the prognosis of metastatic breast cancer. Younger patients, while facing a diagnosis of metastatic disease, often have a longer life expectancy compared to older patients. Furthermore, access to high-quality healthcare and support systems can significantly impact outcomes. For example, patients with greater socioeconomic resources might have better access to advanced treatments and supportive care, potentially leading to improved survival.
Treatment Response
The response to initial treatment regimens is a crucial prognostic factor. Patients who respond well to initial therapies, demonstrating a reduction in tumor burden or stabilization of disease, generally have a better prognosis than those who do not respond or whose disease progresses rapidly. A complete or partial response to chemotherapy or targeted therapies is often associated with longer survival times.
For instance, a patient whose tumor shrinks significantly after chemotherapy might have a more favorable prognosis compared to a patient whose tumor continues to grow despite treatment.
Navigating the prognosis of metastatic breast cancer can be tough, but focusing on healthy lifestyle choices can make a real difference. While research is ongoing, incorporating foods high in creatine, like red meat and fish ( foods high in creatine ), might potentially offer some support in maintaining muscle strength and overall well-being. Ultimately, the prognosis for metastatic breast cancer is complex and varies greatly, but proactive steps like a balanced diet can contribute to a better quality of life for those facing this challenge.
Genetic Markers
Genetic markers provide a more detailed understanding of the disease’s characteristics and potential response to treatments. Specific genetic mutations or alterations can be used to tailor treatment strategies and predict outcomes. For instance, the presence of specific mutations in genes like BRCA1/2 can influence treatment decisions and predict a potential for response to PARP inhibitors. These genetic analyses are becoming increasingly important in guiding treatment choices and anticipating prognosis.
Summary Table of Prognostic Factors
| Factor | Assessment Method | Impact on Survival | Example |
|---|---|---|---|
| Tumor Grade | Pathological examination of tumor tissue | Higher grade tumors generally correlate with poorer prognosis. | High-grade ductal carcinoma in situ (DCIS) has a worse prognosis than low-grade DCIS. |
| Tumor Size | Imaging studies (e.g., MRI, CT) | Larger tumors are often associated with more advanced disease and a shorter survival time. | A tumor measuring 5 cm has a worse prognosis than a tumor measuring 2 cm. |
| Patient Age | Patient history | Younger patients often have a longer life expectancy compared to older patients. | A 40-year-old patient has a potentially better prognosis than an 80-year-old patient. |
| Treatment Response | Monitoring of tumor response during treatment | Patients who respond well to initial therapies have a better prognosis. | A patient whose tumor shrinks significantly after chemotherapy has a better prognosis than a patient whose tumor continues to grow. |
| Genetic Markers | Molecular testing (e.g., PCR, FISH) | Specific genetic alterations can impact treatment options and predict outcomes. | A patient with HER2 amplification might benefit from HER2-targeted therapies, potentially improving survival. |
Treatment Approaches and Prognosis
Navigating metastatic breast cancer requires a personalized approach to treatment. The choice of treatment, and its impact on prognosis, hinges on factors such as the specific type of breast cancer, the extent of metastasis, the patient’s overall health, and the presence of any other underlying conditions. Different treatments work in different ways and each comes with a unique set of potential side effects.Understanding the various treatment options and their respective effects on prognosis is crucial for both patients and their healthcare providers in making informed decisions.
The goal is not only to manage symptoms but also to prolong life and improve quality of life.
Treatment Options for Metastatic Breast Cancer
A range of treatment options are available for metastatic breast cancer, each with its own mechanism of action and potential side effects. These options are frequently combined to maximize effectiveness. The most common approaches include:
- Targeted Therapy: These drugs specifically target cancer cells’ genetic or biochemical vulnerabilities. For instance, drugs like lapatinib and trastuzumab are designed to inhibit specific proteins crucial for cancer growth in HER2-positive breast cancer. This approach often leads to better outcomes in patients with specific genetic markers.
- Chemotherapy: This approach uses powerful drugs to kill cancer cells throughout the body. Chemotherapy regimens can vary greatly depending on the specific cancer type and stage. The effectiveness and potential side effects can vary significantly from patient to patient.
- Hormonal Therapy: This approach targets hormones that fuel the growth of hormone receptor-positive breast cancers. Drugs like tamoxifen and aromatase inhibitors are commonly used to block or reduce the production of these hormones. The success of hormonal therapy hinges on the sensitivity of the tumor to hormones.
- Immunotherapy: This approach utilizes the body’s immune system to fight cancer cells. Immune checkpoint inhibitors are increasingly used in metastatic breast cancer to stimulate the immune response against the cancer. The response to immunotherapy varies widely and is currently under active research.
- Radiation Therapy: This approach uses high-energy radiation to shrink or destroy tumors. Radiation therapy is often used in combination with other treatments, or to alleviate symptoms caused by bone metastasis. The extent and efficacy of radiation therapy depend on the specific location of the metastases.
Impact of Treatment Choices on Prognosis
The effectiveness of a treatment directly impacts the prognosis for metastatic breast cancer. A treatment that successfully controls tumor growth, reduces symptoms, and extends survival will have a positive impact on prognosis. The specific impact of each treatment will depend on the individual characteristics of the cancer, the patient’s health status, and the combination of therapies utilized.
Comparison of Treatment Regimens
| Treatment | Mechanism of Action | Potential Side Effects | Impact on Prognosis |
|---|---|---|---|
| Targeted Therapy (e.g., Trastuzumab) | Targets specific cancer-driving proteins. | Fatigue, nausea, diarrhea, skin rashes. | Can significantly improve survival in HER2-positive breast cancer, often in combination with chemotherapy. |
| Chemotherapy (e.g., Taxanes) | Kills rapidly dividing cancer cells throughout the body. | Hair loss, nausea, vomiting, fatigue, neuropathy. | Can prolong survival and reduce tumor burden, often as part of a combination regimen. |
| Hormonal Therapy (e.g., Tamoxifen) | Blocks or reduces the production of hormones that fuel tumor growth. | Hot flashes, vaginal dryness, mood changes. | Can improve survival in hormone receptor-positive breast cancer, often used in combination with other therapies. |
| Immunotherapy (e.g., Immune checkpoint inhibitors) | Stimulates the immune system to fight cancer cells. | Fatigue, skin rashes, immune-related side effects (e.g., colitis). | Show promise in some patients, especially those with specific biomarkers. Ongoing research is needed. |
| Radiation Therapy | Uses high-energy radiation to shrink or destroy tumors. | Skin reactions, fatigue, and local side effects depending on the area treated. | Can be used to control pain, reduce tumor size, or improve symptoms in specific cases. |
Prognostic Models and Tools
Navigating the complexities of metastatic breast cancer requires tools to predict potential outcomes and tailor treatment strategies. Prognostic models play a crucial role in this process, helping oncologists and patients understand the likelihood of disease progression, response to therapy, and overall survival. These models consider a multitude of factors, from the initial tumor characteristics to the patient’s overall health.
Understanding these models empowers informed decision-making and realistic expectations for the future.
Existing Prognostic Models, Metastatic breast cancer prognosis
Various prognostic models exist for metastatic breast cancer, each attempting to predict patient outcomes with varying degrees of accuracy. These models typically incorporate clinical data, tumor characteristics, and treatment response. A critical aspect is the ability of these models to adapt and incorporate new data and treatment advancements.
Key Factors in Prognostic Models
Prognostic models for metastatic breast cancer typically integrate several factors, each contributing to a comprehensive understanding of the disease’s trajectory. These factors encompass both initial characteristics of the tumor, such as the histological subtype and grade, as well as the patient’s clinical presentation, such as age, performance status, and prior treatment history. The presence of specific genetic markers, such as HER2 status or hormone receptor status, are also frequently included.
Furthermore, factors like the site of metastasis and the response to initial treatment also play a significant role in predicting future outcomes.
Using a Model: A Case Study
Consider a patient diagnosed with metastatic breast cancer, a HER2-positive subtype. Their initial treatment regimen demonstrates a partial response. Utilizing a prognostic model incorporating these factors, along with their age and overall health, the model predicts a median survival time of 3 years. This prediction is a valuable tool for the patient and their physician, offering realistic expectations and facilitating discussions about treatment options and potential outcomes.
Limitations of Prognostic Models
It is essential to acknowledge the limitations of prognostic models. No model can perfectly predict the future, and the predictions are often estimates based on historical data. Factors such as the specific treatment received, adherence to treatment plans, and individual patient responses can all influence outcomes beyond the scope of a model. Additionally, the models often rely on data from large, retrospective studies, and may not always reflect the current, rapidly evolving landscape of treatments and research.
The accuracy of these predictions also depends on the quality and comprehensiveness of the data input into the model.
Table of Prognostic Models
| Model Name | Key Factors Included | Accuracy | Limitations |
|---|---|---|---|
| PAM50 | Gene expression profiling | Moderate | Limited applicability in metastatic settings; not consistently validated across different populations |
| REMARK | Clinical and pathologic features, including hormone receptor status, HER2 status, and tumor size | Moderate | May not account for newer therapies or specific molecular subtypes |
| International Metastatic Breast Cancer Database (IMDC) | Clinical factors like age, performance status, and response to prior therapies | Moderate to high | Can be less precise in predicting outcomes for specific subtypes or treatment regimens |
Patient Experience and Prognosis

Living with metastatic breast cancer is profoundly challenging, impacting not only physical health but also emotional well-being and the entire fabric of a patient’s life. The diagnosis often triggers a cascade of complex emotions, including fear, anxiety, and grief. Understanding the interplay between these emotional factors and the disease’s progression is crucial for developing effective support strategies. This journey requires navigating treatment plans, side effects, and the evolving nature of the disease, demanding resilience and adaptability.The experience of metastatic breast cancer is intensely personal, with diverse responses to the diagnosis and its implications.
The prognosis is multifaceted, encompassing not only the biological aspects of the disease but also the patient’s emotional state, support network, and adherence to treatment.
Impact of the Diagnosis on Patients’ Lives
The diagnosis of metastatic breast cancer profoundly alters a patient’s life trajectory. It necessitates a shift in priorities, impacting work, relationships, and daily routines. Financial concerns, emotional distress, and the uncertainty surrounding future possibilities are common challenges. The experience is unique to each individual, but a shared sense of vulnerability and fear is often present.
Psychological Factors and Support Systems
Psychological factors play a significant role in influencing prognosis. Patients facing this diagnosis often experience significant emotional distress, including anxiety, depression, and fear of the unknown. Strong support systems, including family, friends, and healthcare professionals, can significantly buffer these negative impacts. Access to mental health services and support groups can be crucial for managing the emotional burden.
Patient Adherence to Treatment
Adherence to treatment protocols is a critical factor in influencing prognosis. Patients must actively participate in their care, understanding treatment regimens and potential side effects. This often requires strong communication with their healthcare team and a proactive approach to managing potential challenges. Factors like access to information, transportation, and financial resources can all influence treatment adherence. Effective communication and shared decision-making between patients and healthcare professionals are essential for successful outcomes.
Importance of Quality of Life
Quality of life (QOL) is a crucial component of metastatic breast cancer prognosis. Treatment regimens, while vital for extending survival, can often cause significant side effects that affect a patient’s well-being. Prioritizing QOL involves addressing physical discomfort, emotional distress, and social isolation. This often requires a multidisciplinary approach, including pain management, psychological support, and social work intervention.
Ultimately, a focus on maintaining a good QOL alongside treatment efforts is vital.
Resources for Patient Support and Information
| Resource | Description | Contact Information |
|---|---|---|
| National Breast Cancer Foundation | Provides information, support, and resources for breast cancer patients and their families. | (Information on their website) |
| American Cancer Society | Offers comprehensive information and support services for cancer patients and their families. | (Information on their website) |
| The Susan G. Komen Foundation | Focuses on breast cancer research, prevention, and patient support. | (Information on their website) |
| Metastatic Breast Cancer Network | Provides specific support and information for patients with metastatic breast cancer. | (Information on their website) |
Future Directions in Prognosis Research: Metastatic Breast Cancer Prognosis
Navigating the complexities of metastatic breast cancer requires a deep understanding of its progression and outcomes. Current prognostic tools, while valuable, often fall short in predicting individual patient trajectories. This gap fuels ongoing research aimed at refining prognostic models and tailoring treatment strategies for optimal patient care. Advancements in technology and personalized medicine promise a future where prognostic accuracy is enhanced, and treatment plans are more precisely aligned with individual patient needs.Ongoing research is actively exploring new avenues to improve prognostic accuracy and tailor treatments.
This includes the development of sophisticated algorithms and the incorporation of novel biomarkers. By analyzing vast datasets and identifying subtle patterns, researchers are striving to create more predictive models. These models could provide crucial insights into patient response to therapies and survival rates, allowing for more informed decisions about treatment plans.
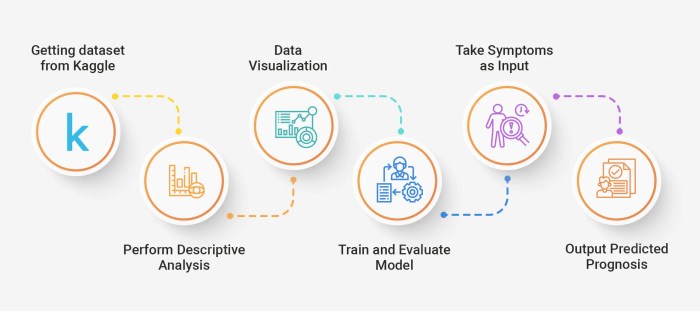
Developing Improved Prognostic Tools and Models
Researchers are actively developing and refining prognostic models for metastatic breast cancer. These models leverage sophisticated statistical techniques and machine learning algorithms to analyze complex data, such as genomic profiles, tumor characteristics, and patient demographics. The goal is to create tools that accurately predict the likelihood of disease progression and response to treatment. One approach involves integrating multiple data points, including protein expression levels and genetic mutations, into a single model to provide a comprehensive picture of the disease.
The Role of New Technologies
Advances in genomic sequencing, proteomics, and imaging technologies are revolutionizing the understanding of metastatic breast cancer. These technologies allow for the identification of specific biomarkers, mutations, and molecular pathways associated with disease progression and response to therapy. For example, advanced imaging techniques like PET scans can reveal the extent and spread of the disease with greater precision, offering insights into tumor burden and treatment efficacy.
The integration of these data into prognostic models promises to lead to more accurate predictions and individualized treatment strategies.
Personalized Medicine and Tailored Treatment
Personalized medicine holds immense potential in the realm of metastatic breast cancer. By identifying specific genetic mutations and molecular characteristics in individual patients, clinicians can select the most effective treatment strategies. For example, targeted therapies tailored to specific genetic alterations can improve outcomes for patients with those mutations. The integration of genomic information with clinical data, such as age, lifestyle, and other medical conditions, will likely provide a more comprehensive understanding of individual patient responses to treatments, paving the way for optimized therapeutic approaches.
Current Research Projects
This table highlights ongoing research projects aimed at improving prognostic models for metastatic breast cancer. The diverse approaches reflect the multifaceted nature of the disease and the need for comprehensive strategies.
| Research Area | Description | Lead Institution |
|---|---|---|
| Integration of Genomic and Clinical Data | Developing a model that integrates genomic profiles, clinical characteristics, and treatment response to predict patient outcomes in metastatic breast cancer. | University of California, San Francisco |
| Novel Biomarker Discovery | Identifying novel blood-based biomarkers to predict disease progression and treatment response in metastatic breast cancer. | National Cancer Institute |
| Advanced Imaging and Prognosis | Utilizing advanced imaging techniques, such as PET/CT, to refine prognostic models for metastatic breast cancer, incorporating tumor burden and metabolic activity into predictions. | Memorial Sloan Kettering Cancer Center |
| AI-driven Prognostic Models | Developing artificial intelligence algorithms to analyze large datasets of genomic and clinical data to predict patient outcomes and identify optimal treatment strategies. | Stanford University |
Last Word
In conclusion, metastatic breast cancer prognosis is a multifaceted concept, influenced by a range of factors. While existing models and tools offer valuable insights, their limitations highlight the ongoing need for research. Ultimately, a personalized approach to treatment, coupled with patient support, plays a vital role in optimizing outcomes and improving the quality of life for those facing this challenging diagnosis.
This exploration offers a detailed understanding of the complexities involved, from the initial diagnosis to the ongoing research aiming to improve prognoses and treatment strategies.


Leave a Reply