Ear infection and covid 19 – Ear infection and COVID-19: Understanding the potential connections between these two common health concerns is crucial. Ear infections, often caused by bacteria or viruses, can manifest in various ways, ranging from mild discomfort to severe pain. COVID-19, while primarily affecting the respiratory system, has shown potential links to a wider range of health issues, including ear problems.
This comprehensive exploration delves into the intricate relationship between ear infections and COVID-19, examining potential symptoms, diagnosis, treatment strategies, and preventive measures. We’ll also discuss the potential long-term effects.
This article will examine the potential impact of COVID-19 on ear infections, covering the potential for new symptoms, unique treatment considerations, and the importance of timely diagnosis. We’ll explore the potential mechanisms by which COVID-19 could affect the ear, as well as potential treatment strategies, including the critical need for preventative measures and ongoing monitoring. Tables will be used to visually compare and contrast different aspects of the two conditions.
Ear Infections and COVID-19
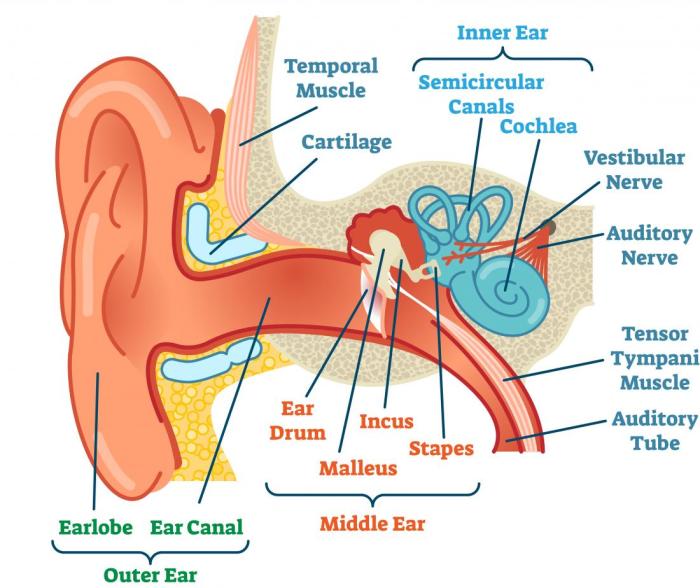
Ear infections, a common ailment affecting people of all ages, are often accompanied by discomfort and sometimes, more serious complications. Understanding the different types, causes, and treatment options is crucial for managing these infections effectively. While the relationship between ear infections and COVID-19 is still being investigated, it’s important to have a comprehensive understanding of both conditions.Ear infections, or otitis, are characterized by inflammation of the middle ear.
This inflammation can be caused by various factors, and understanding these causes can help in preventing and treating them. In many cases, a bacterial or viral infection is the root cause, and recognizing the signs and symptoms is vital for prompt medical intervention.
Types of Ear Infections
Ear infections encompass various types, each with its own characteristics. Knowing the specific type can guide appropriate treatment strategies. Common types include acute otitis media (AOM), otitis externa (swimmer’s ear), and chronic otitis media.
While ear infections and COVID-19 can sometimes overlap, it’s important to remember that stress can also play a significant role in overall health. For instance, researchers are still exploring how stress might impact the body’s response to ear infections or COVID-19 symptoms, potentially leading to unexpected health complications. Have you ever wondered if stress can directly trigger seizures?
Exploring that connection further could help us understand how to better manage potential health issues. Fortunately, understanding the potential link between stress and ear infections/COVID-19 symptoms is crucial for developing effective treatments and preventative strategies. This could include looking into things like can stress cause seizures to see if stress is a factor. Further research is crucial to gain a deeper understanding of these interlinked health concerns.
Symptoms of Ear Infections
Recognizing the symptoms of an ear infection is essential for timely medical intervention. Symptoms can vary depending on the type and severity of the infection. Common symptoms include ear pain, often described as throbbing or aching, fever, hearing loss, and in some cases, a discharge from the ear. Infants may exhibit symptoms such as irritability, difficulty feeding, and pulling at the ear.
Causes of Ear Infections
Ear infections can stem from various sources, including bacterial and viral pathogens. Bacterial infections are a common cause, with Streptococcus pneumoniae and Haemophilus influenzae being frequent culprits. Viral infections, like those causing the common cold, can also lead to ear infections. Blockages in the Eustachian tube, which connects the middle ear to the back of the throat, can also create a conducive environment for infections to develop.
Ever wondered if an ear infection could be linked to COVID-19? While the exact connection isn’t fully understood, some studies suggest a potential correlation. Choosing the right protein powder mix, like whether to mix it with milk or water, might seem trivial compared to a potential health concern like an ear infection, but optimal nutrition can support your body’s natural defenses.
For a deeper dive into the best way to mix protein powder, check out this helpful guide on protein powder with milk or water. Ultimately, more research is needed to definitively clarify the link between ear infections and COVID-19.
Treatment Approaches for Ear Infections
The treatment approach for ear infections depends on the type and severity of the infection. For bacterial infections, antibiotics are often prescribed. In cases of viral infections, supportive care, such as pain relievers and rest, is typically recommended. In some situations, a combination of antibiotics and other medications may be required. The selection of antibiotics is based on the specific bacteria causing the infection, and careful consideration is given to antibiotic resistance.
Prevalence of Ear Infections
Ear infections are relatively common, particularly in young children. Studies show a significant prevalence of ear infections in the general population, with variations based on factors like age, geographic location, and overall health status. For instance, young children are more susceptible to ear infections due to the immaturity of their Eustachian tubes. This susceptibility, along with other contributing factors, makes ear infections a significant concern for public health.
Ear Infection Overview
| Infection Type | Symptoms | Typical Treatment |
|---|---|---|
| Acute Otitis Media (AOM) | Earache, fever, hearing loss, possible discharge | Antibiotics (if bacterial), pain relievers, rest |
| Otitis Externa (Swimmer’s Ear) | Earache, itching, discharge, swelling | Ear drops, pain relievers, keeping the ear dry |
| Chronic Otitis Media | Persistent earache, discharge, hearing loss, possible perforation of eardrum | Antibiotics, possibly surgery (tympanostomy tubes) |
COVID-19’s Impact on the Ear
The COVID-19 pandemic has presented numerous health challenges, and while its primary effects are often associated with respiratory systems, emerging evidence suggests a potential connection between the virus and ear problems. Understanding this connection is crucial for better patient care and public health strategies. Early research and reported cases highlight the need for further investigation into the potential links between COVID-19 and ear-related issues.Emerging data indicates that COVID-19 infection might influence the ear in various ways, potentially leading to a range of conditions.
While the precise mechanisms aren’t fully understood, the virus’s interaction with the body’s immune system and its ability to affect different tissues are factors that could contribute to ear complications. Further studies are vital to unravel the complexity of this relationship.
Potential Links Between COVID-19 and Ear Problems
COVID-19’s impact on the auditory system is a topic of ongoing investigation. The virus can potentially cause inflammation and damage to tissues in the ear, leading to a variety of ear-related problems. This can be influenced by factors like the severity of the initial COVID-19 infection, individual immune responses, and pre-existing health conditions.
Documented Cases and Studies
Although a direct causal link between COVID-19 and specific ear conditions is still being researched, anecdotal reports and some preliminary studies have suggested potential associations. More robust studies are needed to confirm these findings and understand the specific mechanisms involved. These early reports highlight the need for further research and dedicated studies focusing on the relationship between COVID-19 and ear problems.
Comparison of Ear Infection Rates Before and During the Pandemic
Reliable data on ear infection rates specifically before and during the COVID-19 pandemic is limited and often varies depending on geographic location and reporting methods. Comparing ear infection rates across different time periods requires meticulous analysis of various factors, such as the overall health of the population, access to healthcare, and reporting practices. Changes in these factors can affect the rates, making direct comparisons complex.
Potential Mechanisms of COVID-19’s Impact on the Ear
Several potential mechanisms could explain how COVID-19 might affect the ear. The virus’s ability to infect and potentially damage cells in the ear, including the middle ear and inner ear structures, is a primary consideration. Additionally, the inflammatory response triggered by the infection could contribute to ear problems. The virus’s impact on the immune system and its ability to cause inflammation in other parts of the body are also potential factors.
Comparison of Symptoms
| Symptom | Typical Ear Infection | Potentially COVID-19 Related Ear Issues |
|---|---|---|
| Earache | Common, often sharp or dull | Possible, but may not be the primary symptom |
| Hearing Loss | Possible, but not always present | Possible, particularly with inner ear involvement |
| Ear Drainage | Often present, may be pus or fluid | Possible, but not a defining symptom |
| Vertigo/Dizziness | Rare, possibly related to inner ear infection | Possible, potentially associated with inner ear inflammation or other neurological complications |
| Tinnitus | Possible, but not always present | Possible, potentially linked to inner ear issues |
Note: This table provides a general comparison. Symptoms can vary greatly depending on the individual and the specific condition. A proper diagnosis by a healthcare professional is essential.
Potential Symptoms and Diagnosis

Navigating the complexities of ear infections and COVID-19 requires a keen understanding of overlapping symptoms and diagnostic nuances. Distinguishing between these conditions can be challenging, highlighting the critical role of a thorough medical evaluation. Accurate diagnosis is essential for appropriate treatment and to prevent potential complications.
Common Overlapping Symptoms
Symptoms of ear infections and COVID-19 can sometimes overlap, making accurate diagnosis difficult. Both conditions can present with pain, pressure, and a feeling of fullness in the ear. A stuffy nose, a common COVID-19 symptom, can also accompany ear infections, making differentiation even more challenging. Other potential overlaps include fever, headache, and fatigue.
Diagnostic Methods for Ear Infections
Diagnosing ear infections involves a combination of physical examination and potentially additional tests. A physical examination of the ear canal and eardrum is often the first step. Otoscopy, a procedure using an otoscope to visualize the ear canal and eardrum, allows the healthcare provider to identify signs of infection, such as redness, swelling, or fluid buildup behind the eardrum.
Additional tests, such as tympanometry, may be used to assess the function of the eardrum and middle ear.
Distinguishing Between COVID-19 and Other Ear Infection Causes, Ear infection and covid 19
Differentiating between COVID-19-related ear symptoms and other causes of ear infections requires a comprehensive approach. Consideration of the patient’s complete medical history, including recent exposure to individuals with COVID-19, is crucial. The presence of other respiratory symptoms, such as cough, sore throat, or runny nose, along with a history of recent travel or contact with infected individuals, can strongly suggest a COVID-19-related ear condition.
Importance of Timely Diagnosis and Treatment
Prompt diagnosis and treatment are crucial for both ear infections and COVID-19. Untreated ear infections can lead to complications such as hearing loss, ruptured eardrums, and mastoiditis, an infection of the bone behind the ear. Similarly, delayed treatment of COVID-19 can result in severe illness and potential long-term health issues. Early intervention significantly improves outcomes and prevents potential complications.
Potential Symptoms Table
| Symptom | Severity (Mild/Moderate/Severe) | Possible Causes (Ear Infection vs. COVID-19) |
|---|---|---|
| Ear pain | Moderate | Both. Ear infections can cause significant pain, often described as a throbbing or aching sensation. COVID-19 related ear pain is less common, but possible. |
| Ear fullness | Mild to Moderate | Both. A feeling of pressure or fullness in the ear can occur with both conditions. |
| Hearing loss | Mild to Severe | Ear infection: Potential if the infection causes fluid buildup or damage to the eardrum. COVID-19: Possible, but less common than other symptoms. |
| Fever | Mild to Moderate | Both. Fever is a common symptom of both conditions, though other symptoms may aid in differentiation. |
| Cough | Mild to Severe | COVID-19: A primary symptom. Ear infections: Less common, but a possible symptom in some cases. |
Treatment Strategies and Considerations
Treating ear infections, especially when coupled with COVID-19, requires careful consideration of potential interactions and individualized approaches. The standard treatments for ear infections, while generally safe and effective, may need adjustments based on the patient’s overall health status and concurrent COVID-19 infection. Understanding the nuances of these interactions is crucial for optimal patient outcomes.Effective management of ear infections necessitates a multifaceted approach that addresses both the infection itself and the potential impact of a co-existing COVID-19 infection.
This involves a thorough evaluation of the patient’s medical history, current symptoms, and the severity of both conditions. The choice of treatment will depend on factors like the type of ear infection, the patient’s age and overall health, and the presence of any other underlying medical conditions.
Treatment Approaches for Ear Infections
Various treatment strategies are available for ear infections, ranging from over-the-counter pain relievers to antibiotic or antiviral medications. The specific approach depends on the type of infection and its severity. For example, uncomplicated acute otitis media (AOM) might be managed with pain relief and close monitoring, while more severe or recurrent cases might require antibiotic therapy.
Ever wonder if an ear infection could be linked to COVID-19? While the exact connection isn’t fully understood, some research suggests a possible correlation. One key element in managing potential complications is understanding how to boost metabolism, as a healthy metabolism can aid in the body’s natural healing processes. For detailed information on strategies to improve your metabolic rate, check out this helpful guide on how to boost metabolism.
Regardless of the exact relationship, prioritizing overall health, including immune support, remains crucial in managing potential ear infections and their possible links to COVID-19.
Safety and Efficacy of Treatments
The safety and efficacy of treatments for ear infections need to be assessed in the context of a potential COVID-19 infection. Some medications used to treat ear infections may have potential interactions with COVID-19 medications, and this needs to be carefully evaluated. For example, certain antibiotics might interfere with the metabolism or effectiveness of some antiviral drugs used to treat COVID-19.
Managing Ear Infections During a COVID-19 Outbreak
Managing ear infections during a COVID-19 outbreak necessitates careful attention to resource allocation and infection control measures. Healthcare providers need to prioritize patient safety while ensuring timely and appropriate treatment. This might involve adjusting clinic protocols to reduce potential transmission and maximizing the use of telehealth or remote monitoring options, especially for mild cases.
Precautions and Safety Measures
Comprehensive precautions and safety measures are crucial for individuals with both ear infections and COVID-19. This includes rigorous hand hygiene, maintaining social distancing, and wearing appropriate personal protective equipment (PPE) when necessary. Adherence to these precautions helps minimize the risk of spreading either infection to others. Furthermore, individuals should isolate themselves if symptomatic to prevent potential transmission.
Comparison of Treatment Options
| Treatment Option | Potential Interactions with COVID-19 Therapies | Safety Considerations | Efficacy |
|---|---|---|---|
| Over-the-counter pain relievers (e.g., ibuprofen, acetaminophen) | Generally safe and unlikely to interact with COVID-19 medications. | Can be used for mild cases, but may not address the underlying infection. | Effective in reducing pain and discomfort. |
| Antibiotics (e.g., amoxicillin) | Potential for interactions with certain antiviral medications used for COVID-19; careful monitoring and adjustment of dosages may be required. | Should be prescribed only when clinically indicated, as overuse can lead to antibiotic resistance. | Effective in treating bacterial infections, but not for viral infections like COVID-19. |
| Antiviral medications (e.g., for COVID-19) | May interact with some antibiotics, potentially reducing their effectiveness or increasing side effects; careful consideration of drug interactions is paramount. | Should be used only as directed by a healthcare professional and in the appropriate clinical context. | Effectiveness in treating COVID-19 depends on the specific drug and the stage of the infection. |
Prevention and Public Health Measures
Protecting ourselves and our communities from both ear infections and COVID-19 requires a multifaceted approach. This involves understanding the spread of these infections and implementing effective preventive measures. Proactive strategies, including hand hygiene, social distancing, and vaccination, play a critical role in minimizing the risk of contracting and spreading these illnesses.Effective prevention is crucial, not just for individual well-being but also for the broader public health picture.
By understanding the mechanisms of transmission and actively employing preventive strategies, we can significantly reduce the burden of these illnesses on individuals and healthcare systems. This approach is particularly relevant in a pandemic context, where maintaining community health is paramount.
Hand Hygiene Practices
Maintaining meticulous hand hygiene is a fundamental aspect of preventing the spread of both ear infections and COVID-19. Germs, including those responsible for ear infections, can easily be transmitted through contaminated hands. Regular and thorough handwashing is vital in reducing the risk of infection. Proper handwashing techniques, which include using soap and water for at least 20 seconds, are essential to remove pathogens.
Social Distancing Strategies
Social distancing measures are crucial in reducing the transmission of both ear infections and COVID-19. These measures aim to limit close contact between individuals, thereby minimizing the potential for the spread of infectious agents. Maintaining a safe physical distance, particularly in crowded areas, significantly reduces the risk of exposure to pathogens. This strategy is especially important in settings where close proximity is unavoidable.
Vaccination Strategies
Vaccination remains a powerful tool in preventing infectious diseases, including both ear infections and COVID-19. Vaccines stimulate the body’s immune response, creating antibodies that provide protection against the pathogens. Vaccines are often the most effective and safest approach to prevent severe illness and hospitalization. Individuals should consult with their healthcare providers to understand the recommended vaccination schedule and any potential risks or benefits.
Public Health Initiatives
Public health initiatives play a critical role in mitigating the impact of both ear infections and COVID-19 on communities. These initiatives focus on educating the public about preventive measures, promoting vaccination campaigns, and implementing policies to reduce the spread of infections. Effective public health campaigns often include targeted messaging to specific demographics and geographical areas.
Preventive Measures Summary
- Hand Hygiene: Wash hands frequently with soap and water for at least 20 seconds, especially after touching surfaces or interacting with others. Use hand sanitizer with at least 60% alcohol content when soap and water are unavailable.
- Social Distancing: Maintain a safe physical distance from others, particularly in crowded areas. Avoid close contact and consider wearing a mask in public spaces.
- Vaccination: Adhere to recommended vaccination schedules for both COVID-19 and other preventable illnesses, as appropriate.
- Public Health Initiatives: Follow guidelines and recommendations from public health organizations to protect yourself and your community.
- Environmental Hygiene: Regularly clean and disinfect frequently touched surfaces like doorknobs, light switches, and countertops to reduce the presence of pathogens.
- Hygiene for Children: Teach children proper handwashing techniques, especially before meals and after using the restroom. Supervise their interactions to limit potential exposure to ear infections and other illnesses.
Long-Term Effects and Complications: Ear Infection And Covid 19
Ear infections, while often treatable, can sometimes have lasting consequences. Understanding these potential complications is crucial for proactive management and ensuring optimal health outcomes. This section will delve into the long-term effects of ear infections, both in isolation and in the context of a concurrent COVID-19 infection. Proper diagnosis and timely treatment are paramount to mitigating these risks.
Potential Long-Term Effects of Ear Infections (Independent of COVID-19)
Ear infections, if left untreated or inadequately treated, can lead to a range of long-term complications. These complications can affect hearing, balance, and even the surrounding structures of the ear. Early intervention significantly reduces the likelihood of these issues developing.
- Hearing Loss: Chronic or recurring ear infections can damage the delicate structures within the ear, leading to permanent hearing loss. The degree of hearing loss varies depending on the severity and duration of the infection. In some cases, hearing loss may be mild and manageable with hearing aids, while in others, it may be significant and require more intensive intervention.
- Balance Disorders: Ear infections can disrupt the delicate balance mechanisms within the inner ear. This can manifest as dizziness, vertigo, and difficulty maintaining balance. These issues can significantly impact daily activities and require careful management.
- Facial Nerve Palsies: In rare cases, severe ear infections can lead to inflammation and damage to the facial nerve, resulting in facial paralysis. This can affect the ability to control facial muscles and expressions.
- Mastoiditis: If an ear infection spreads to the mastoid bone behind the ear, it can cause mastoiditis, a potentially serious infection requiring further medical intervention. This condition can lead to bone damage and significant discomfort.
Potential Complications from Untreated or Inadequately Treated Ear Infections
Untreated or inadequately treated ear infections can lead to more severe and prolonged health issues. Prompt and appropriate medical attention is crucial to prevent the development of these complications.
- Chronic Otitis Media: Recurring ear infections can lead to chronic otitis media, a condition characterized by persistent inflammation of the middle ear. This can cause persistent discomfort, hearing loss, and potential damage to the eardrum.
- Cholesteatoma: In some cases, chronic ear infections can lead to the formation of a cholesteatoma, a benign but potentially destructive growth of skin cells in the middle ear. This growth can erode surrounding bone structures and potentially lead to hearing loss or facial nerve complications.
Long-Term Complications in the Context of COVID-19
The relationship between ear infections and COVID-19 is an area of ongoing research. While the exact mechanisms are not fully understood, there is a potential link between the two. COVID-19 can cause inflammation and damage to various parts of the body, potentially exacerbating pre-existing ear infections or increasing the risk of new ones.
- Increased Risk of Infection: Individuals with weakened immune systems due to COVID-19 may be more susceptible to ear infections.
- Delayed Healing: The presence of a COVID-19 infection might impact the body’s ability to heal from an ear infection, potentially leading to a prolonged recovery period.
Importance of Ongoing Monitoring and Follow-up Care
Ongoing monitoring and follow-up care are crucial for individuals with ear infections, regardless of any other underlying conditions. Regular check-ups allow healthcare providers to track the progress of the infection, assess the effectiveness of treatment, and identify any potential complications early on.
Table of Potential Long-Term Complications
| Severity of Infection | Potential Long-Term Complications |
|---|---|
| Mild | Hearing loss (minor), temporary balance issues |
| Moderate | Chronic otitis media, moderate hearing loss, facial nerve involvement (rare) |
| Severe | Significant hearing loss, cholesteatoma, mastoiditis, facial nerve paralysis, balance disorders (severe) |
Conclusion
In conclusion, the relationship between ear infections and COVID-19 is complex and warrants careful consideration. While definitive links between the two conditions are still being investigated, it’s clear that understanding potential interactions is crucial for effective diagnosis and treatment. This article has highlighted the potential for shared symptoms, unique treatment challenges, and the importance of preventative measures. Continued research and vigilance are essential for navigating the evolving landscape of these health concerns.




