Pelvic inflammatory disease pid – Pelvic inflammatory disease (PID) is a serious infection that affects the female reproductive organs. It can cause a range of symptoms, from mild discomfort to severe pain and complications. Understanding the causes, risk factors, diagnosis, and treatment options for PID is crucial for prevention and management.
This comprehensive guide explores the multifaceted nature of PID, from its common causes, such as bacterial infections, to the potential long-term consequences, including infertility. We’ll also examine the various risk factors, the importance of early detection, and the available treatment options. Prepare to delve into the intricacies of this condition and discover strategies for prevention and support.
Introduction to Pelvic Inflammatory Disease (PID)
Pelvic inflammatory disease (PID) is a serious infection of the female reproductive organs. It’s characterized by inflammation of the uterus, fallopian tubes, and ovaries. Left untreated, PID can lead to significant complications, including infertility and chronic pelvic pain. Understanding the causes, symptoms, and stages of PID is crucial for early diagnosis and effective treatment.PID develops when bacteria ascend from the vagina or cervix into the upper reproductive tract.
This ascent is often facilitated by factors like unprotected sexual intercourse, certain types of intrauterine devices (IUDs), or previous infections. The presence of bacteria, including
- Chlamydia trachomatis* and
- Neisseria gonorrhoeae*, is a major contributing factor, though other bacteria can also be involved.
Common Causes of PID
Factors contributing to the development of PID include sexually transmitted infections (STIs), particularly
- Chlamydia* and
- Gonorrhea*. Other contributing factors include other bacterial infections, intrauterine devices (IUDs), and certain medical procedures. Unprotected sexual activity significantly increases the risk.
Symptoms of PID
PID symptoms can vary significantly in presentation and severity, often appearing subtly in the early stages. This variability can make early diagnosis challenging. Early detection and prompt treatment are essential to prevent long-term complications.
Comparison of PID Symptoms Across Stages
| Symptom | Early Stage | Moderate Stage | Severe Stage |
|---|---|---|---|
| Lower abdominal pain | Mild, intermittent, often vague. May be mistaken for other conditions. | Moderate, persistent, localized pain. Discomfort may radiate to the lower back or groin. | Severe, sharp, constant pain. Pain may be incapacitating and require urgent medical attention. |
| Fever | Possible, but often low-grade or absent. | Moderate fever (101°F-102°F) and chills, often accompanied by other symptoms. | High fever (103°F or higher) with severe chills and sweats. |
| Vaginal discharge | May be slightly unusual in consistency or amount. | Increased vaginal discharge, possibly with an unusual odor or color. | Profuse, foul-smelling vaginal discharge. |
| Nausea and vomiting | Possible, but often mild. | More pronounced nausea and vomiting, potentially indicative of systemic involvement. | Severe nausea and vomiting, potentially accompanied by dehydration. |
| Painful urination | Possible, but often mild. | Increased pain with urination. | Severe pain with urination, potentially indicating complications. |
| Abnormal bleeding | Possible, but may be irregular or spotting. | Heavier or prolonged bleeding, or bleeding between periods. | Excessive bleeding, potentially requiring medical intervention. |
| Tenderness in the lower abdomen | Mild tenderness upon palpation. | Moderate tenderness in the lower abdomen. | Severe tenderness and/or palpable masses in the lower abdomen, indicating inflammation. |
Risk Factors and Predisposing Conditions
Pelvic inflammatory disease (PID) is a serious infection that can lead to long-term complications if left untreated. Understanding the factors that increase a person’s risk is crucial for prevention and early intervention. Recognizing these risks allows individuals and healthcare providers to take proactive steps to minimize the likelihood of developing PID.The risk of developing PID is influenced by various factors, including lifestyle choices, pre-existing medical conditions, and demographic characteristics.
Pelvic inflammatory disease (PID) can be a real pain, affecting women’s reproductive health. It’s important to address it quickly. Sometimes, similar to compulsive behaviors like trichotillomania hair pulling disorder , underlying emotional factors can play a role in the development of chronic pain. Understanding these connections can help women navigate the complexities of PID effectively and seek appropriate care.
Understanding these risk factors is essential for both prevention and treatment strategies.
Factors Increasing PID Risk
Several factors significantly increase the risk of developing PID. These factors highlight the importance of preventative measures and prompt medical attention if symptoms arise.
Pelvic inflammatory disease (PID) can be a real pain, impacting a woman’s overall well-being. It’s important to get it treated promptly, but sometimes other seemingly unrelated issues can also be bothersome. For example, a bug bite on the eyelid, like the ones you can find more info about here , can be distracting and annoying. Ultimately, though, PID needs to remain a top priority for women’s health.
- Sexual Activity:
- Multiple sexual partners significantly increase the risk of contracting sexually transmitted infections (STIs), which are a major cause of PID. Consistent and protected sexual practices, including using condoms, can drastically reduce the risk of infection and PID.
- Unprotected sexual intercourse increases the risk of STIs, significantly raising the likelihood of PID development.
- Early age of sexual debut can also increase the risk of PID due to a higher likelihood of exposure to STIs and a potentially less developed immune response.
- Sexually Transmitted Infections (STIs):
- Certain STIs, like chlamydia and gonorrhea, are primary culprits in the development of PID. These infections can ascend from the genital tract, causing inflammation and damage to the reproductive organs.
- If left untreated, STIs can progress to PID, leading to serious complications. Early detection and treatment of STIs are crucial to preventing PID.
- Neisseria gonorrhoeae and Chlamydia trachomatis are the most common culprits, often co-existing, increasing the risk of PID.
- Intrauterine Devices (IUDs):
- While IUDs are a reliable method of contraception, there is a slightly increased risk of PID in the first few weeks after insertion. This risk is generally low, but it’s essential for women to be aware of this possibility and to seek medical attention promptly if they experience any symptoms.
- Proper insertion technique and follow-up care with a healthcare provider can minimize this risk. Regular check-ups are essential to ensure the IUD remains properly positioned and to monitor for any signs of infection.
Demographic Risk Comparisons
PID risk varies across different demographic groups. Understanding these differences allows for targeted prevention strategies and appropriate healthcare recommendations.
- Age:
- Young women are at higher risk of PID due to factors such as increased sexual activity, earlier sexual debut, and possibly less awareness of preventative measures. However, PID can affect women of any age.
- Gender:
- PID primarily affects women due to the unique anatomy of the female reproductive system. The anatomical pathway allows for easier ascension of bacteria from the lower genital tract to the upper reproductive organs, increasing susceptibility to PID.
Correlation Between Risk Factors and PID Severity
The severity of PID can vary depending on the underlying risk factors.
| Risk Factor | Potential Impact on PID Severity |
|---|---|
| Multiple sexual partners | Increased risk of infection and potentially more severe inflammation |
| History of STIs | Higher chance of recurrent infections and more significant tissue damage |
| IUD use (within first few weeks) | Slightly increased risk of infection, but usually mild and manageable with appropriate treatment |
| Unprotected sex | Higher likelihood of contracting STIs and subsequent PID |
Diagnosis and Treatment Options

Diagnosing pelvic inflammatory disease (PID) requires a combination of clinical evaluation and laboratory tests. Accurate diagnosis is crucial for timely and effective treatment, minimizing potential complications. Treatment options focus on addressing the infection and preventing long-term health issues.
Diagnostic Methods
PID diagnosis often begins with a thorough physical examination, including a pelvic exam. This examination allows the healthcare provider to assess for signs such as tenderness in the lower abdomen, especially in the pelvic area, and abnormal vaginal discharge. Additional physical findings may include fever, pain during sexual intercourse, and pain during urination.
Laboratory Tests, Pelvic inflammatory disease pid
Laboratory tests play a vital role in confirming the suspicion of PID. These tests can help identify the causative bacteria and determine the severity of the infection. Common laboratory tests include:
- Complete Blood Count (CBC): A CBC helps assess the presence of infection by evaluating white blood cell counts, which often increase during an infection.
- Urinalysis: A urinalysis checks for signs of urinary tract infection (UTI), which can sometimes be confused with PID. It also assesses the presence of bacteria in the urine.
- Cultures: Cultures of cervical or vaginal swabs can identify the specific bacteria causing the infection. This is critical for tailoring antibiotic treatment.
- Pregnancy Test: A pregnancy test is essential to rule out pregnancy, as some symptoms of PID can overlap with pregnancy-related conditions.
Treatment Approaches
Effective treatment for PID typically involves antibiotics. The choice of antibiotics depends on the specific bacteria identified in cultures and the patient’s overall health.
- Antibiotics: Antibiotics are the cornerstone of PID treatment. They work by eliminating the bacteria causing the infection. Various antibiotic regimens are used, each tailored to the specific situation. Treatment regimens often include intravenous (IV) antibiotics for severe cases and oral antibiotics for less severe cases.
- Surgical Interventions: Surgical intervention may be necessary in some cases, particularly if there’s evidence of complications such as abscesses or tubal damage. Laparoscopic surgery, a minimally invasive technique, is frequently used for these situations. It allows the surgeon to directly visualize the affected area and drain any abscesses or repair damaged fallopian tubes.
Typical Treatment Duration
The duration of PID treatment varies depending on the severity of the infection and the patient’s response to treatment. Generally, treatment lasts several weeks. A healthcare provider will monitor the patient’s progress and adjust the treatment plan as needed.
Antibiotic Regimens for PID
| Regimen | Antibiotic | Dosage | Duration |
|---|---|---|---|
| Regimen A | Cefotetan + Doxycycline | IV Cefotetan 2g every 12 hours and Oral Doxycycline 100mg twice daily | 14 days |
| Regimen B | Ceftriaxone + Doxycycline | IV Ceftriaxone 250mg once daily and Oral Doxycycline 100mg twice daily | 14 days |
| Regimen C | Clindamycin + Gentamicin | IV Clindamycin 900mg every 8 hours and IV Gentamicin 2mg/kg loading dose, followed by 1.5mg/kg every 8 hours | 14 days |
Note: These are examples of common regimens. Specific antibiotic choices and dosages should be determined by a healthcare provider based on individual circumstances. Dosage adjustments might be necessary for patients with kidney or liver problems.
Complications and Long-Term Effects
Pelvic inflammatory disease (PID) can have serious consequences if left untreated or inadequately treated. The infection can spread, causing damage to reproductive organs and leading to long-term health issues. Understanding these complications is crucial for early diagnosis and effective management.Untreated or poorly treated PID can lead to a cascade of complications, impacting not only reproductive health but overall well-being.
These complications can range from relatively minor discomfort to severe and debilitating conditions that affect quality of life. It’s important to remember that early intervention and appropriate antibiotic treatment are key to minimizing these risks.
Infertility
PID can damage the fallopian tubes, the structures that transport eggs from the ovaries to the uterus. This damage can result in scarring and blockages, preventing the egg and sperm from meeting. This is a significant cause of infertility in women of reproductive age. The severity of the damage directly correlates with the likelihood of experiencing fertility issues.
For example, extensive scarring can completely obstruct the tubes, making pregnancy impossible without medical intervention.
Chronic Pelvic Pain
Chronic pelvic pain is another frequent complication of PID. The inflammation and scarring associated with PID can cause persistent pain in the pelvic region. This pain can range from mild discomfort to severe, debilitating cramps, impacting daily activities and overall well-being. The pain often manifests as a dull ache or sharp twinges, varying in intensity and location. Women may experience this pain during menstruation, sexual intercourse, or even at rest.
Ectopic Pregnancy
A potentially life-threatening complication is the risk of ectopic pregnancy. When PID damages the fallopian tubes, the fertilized egg may implant outside the uterus, typically in the fallopian tube. This is a dangerous condition that requires immediate medical attention. The fertilized egg cannot develop normally in this location, potentially causing severe internal bleeding or rupture of the fallopian tube.
PID Complications by Age Group
The impact of PID on reproductive health can vary based on the age of the affected individual. In younger women, the potential for future fertility issues is significant, especially if the infection is not promptly addressed. Older women, while facing a different set of health concerns, may experience chronic pelvic pain that can impact their daily lives. Both age groups need careful monitoring and timely intervention to minimize long-term effects.
Prevalence of PID Complications
| Complication | Prevalence (estimated, may vary based on study and risk factors) |
|---|---|
| Infertility | 20-40% |
| Chronic Pelvic Pain | 15-30% |
| Ectopic Pregnancy | 5-10% |
Note: These figures are estimates and can be influenced by various factors, including access to healthcare, prompt diagnosis, and treatment effectiveness.
Prevention Strategies and Public Health Initiatives: Pelvic Inflammatory Disease Pid
Pelvic inflammatory disease (PID) is a serious condition that can lead to long-term complications. Fortunately, several strategies can significantly reduce the risk of developing PID. Proactive measures, coupled with public health initiatives, play a crucial role in mitigating the impact of this illness.Effective prevention strategies often involve a combination of individual choices and community-wide efforts. By understanding the risk factors and implementing preventive measures, individuals can greatly reduce their likelihood of contracting PID.
Public health initiatives are vital in raising awareness, promoting healthy behaviors, and ultimately saving lives.
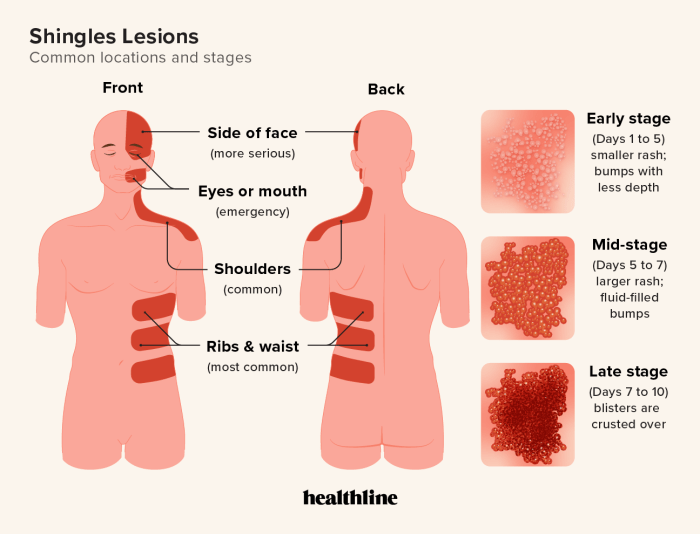
Pelvic inflammatory disease (PID) can be a serious issue, impacting women’s reproductive health. While seemingly unrelated, recent reports of bird flu pediatric cases in the United States, like this one , highlight the importance of understanding and addressing infectious diseases across different demographics. Fortunately, there are effective treatments for PID, which often involve antibiotics and rest.
Preventive Measures Individuals Can Take
Understanding and practicing safe sexual behaviors is paramount in preventing PID. Consistent and correct condom use significantly reduces the transmission of sexually transmitted infections (STIs), which are a major cause of PID. Open communication with sexual partners about STI status and the importance of regular testing is crucial. This fosters a collaborative approach to sexual health and reduces the risk for both partners.
- Safe Sexual Practices: Consistent and correct condom use is a cornerstone of STI prevention. Open communication with partners about sexual health history and STI testing is vital. Mutual respect and understanding regarding sexual health practices are essential.
- Regular STI Screenings: Regular STI screenings are critical for early detection and treatment. This allows for prompt intervention, reducing the risk of PID development. Individuals who are sexually active should discuss STI screening schedules with their healthcare providers.
- Treatment of Existing STIs: Prompt treatment of any existing STIs is essential. Untreated STIs can easily progress to PID, highlighting the importance of seeking medical attention for any suspected infections.
Public Health Campaigns and Awareness
Public health campaigns play a critical role in raising awareness about PID and promoting preventive measures. These campaigns often target at-risk populations and utilize various communication channels, such as educational materials, social media campaigns, and community outreach programs. These campaigns emphasize the importance of early diagnosis, treatment, and prevention.
- Educational Materials: Disseminating educational materials about PID and STI prevention, such as brochures and online resources, can empower individuals with the knowledge needed to make informed decisions. Clear, accessible information is key.
- Community Outreach Programs: Community outreach programs, including workshops and seminars, provide valuable opportunities for individuals to learn about PID and preventive measures in a supportive setting. These programs can offer direct access to healthcare resources and address any concerns.
- Social Media Campaigns: Social media platforms can be utilized to reach wider audiences with important information about PID prevention and treatment. These campaigns can use engaging content to foster discussions and encourage preventative behaviors.
Importance of Regular Checkups and STI Screenings
Regular checkups and STI screenings are vital components of preventive care. Early detection and treatment of STIs can significantly reduce the risk of developing PID. This proactive approach can help individuals maintain their sexual health and overall well-being. Prompt diagnosis and treatment can prevent serious complications.
| Preventive Measure | Effectiveness | Explanation |
|---|---|---|
| Safe Sexual Practices (e.g., condom use) | High | Reduces transmission of STIs significantly. |
| Regular STI Screenings | High | Allows for early detection and treatment, preventing PID. |
| Treatment of Existing STIs | High | Stops the progression of infection to PID. |
| Public Health Campaigns | Moderate to High | Raises awareness and promotes preventive behaviors. |
Patient Experience and Support Systems
Navigating a diagnosis of pelvic inflammatory disease (PID) can be emotionally challenging. The physical discomfort, potential long-term complications, and the uncertainty surrounding treatment can significantly impact a patient’s mental well-being. Understanding the emotional and psychological toll, along with access to appropriate support systems, is crucial for successful management and recovery.Living with PID can be isolating. Fear of the unknown, potential fertility issues, and the need for ongoing medical attention can contribute to feelings of anxiety, depression, and stress.
It’s important to acknowledge the multifaceted impact of this condition on a patient’s life, beyond the immediate physical symptoms.
Emotional and Psychological Impact
The emotional and psychological impact of PID often extends beyond the physical discomfort. Patients may experience feelings of anxiety, fear, and even depression, particularly when facing potential long-term consequences like infertility. These feelings can be compounded by the uncertainty surrounding the diagnosis and treatment options. Recognizing these emotional responses as part of the experience is key to providing comprehensive care.
Support Systems for Individuals with PID
Access to a supportive network is vital during the PID journey. This network can include family, friends, support groups, and healthcare professionals. Support groups offer a safe space for sharing experiences, receiving emotional support, and gaining insights from others facing similar challenges. These groups can provide invaluable emotional comfort and practical advice. A strong support system helps patients feel less isolated and more empowered to manage their condition.
Importance of Patient Education and Access to Healthcare Resources
Comprehensive patient education plays a crucial role in managing PID effectively. Clear and accessible information about the condition, treatment options, potential complications, and preventative measures empowers patients to actively participate in their healthcare. This knowledge helps them make informed decisions and manage their condition effectively. Equally important is easy access to healthcare resources. This includes having readily available information about support groups, local clinics, and relevant specialists.
Patients should be provided with the resources to seek the necessary medical and emotional support.
Creating a Supportive Environment
A supportive environment during diagnosis, treatment, and recovery is critical for positive outcomes. This encompasses not only physical comfort but also emotional support. Open communication between patients and healthcare providers is essential to address concerns and build trust. Healthcare professionals should actively listen to patient experiences, validate their feelings, and offer guidance. This support should extend beyond the medical team to include family, friends, and community resources.
A nurturing environment, both physically and emotionally, is key to successful recovery and long-term well-being.
Illustrative Case Studies (Hypothetical)
Understanding pelvic inflammatory disease (PID) requires examining real-world scenarios. These hypothetical case studies illustrate the range of presentations, diagnostic approaches, and treatment considerations. While not actual patients, they highlight the importance of early intervention and appropriate management for optimal outcomes.Hypothetical cases can help us better understand how PID manifests in different individuals and how variations in symptoms, severity, and predisposing factors impact the diagnostic process and treatment plan.
Case Study 1: A Young Woman with Uncommon Symptoms
A 22-year-old woman, Sarah, presents to her gynecologist complaining of persistent lower abdominal pain, fatigue, and a slight fever. She reports a history of multiple sexual partners and inconsistent use of contraception. These symptoms, while not immediately indicative of PID, warrant further investigation given her risk factors.
Diagnostic Process and Treatment Plan
Initial assessments include a thorough medical history, physical examination, and laboratory tests. The physician will likely order a pelvic exam to assess for signs of inflammation. A urine test, blood tests (including complete blood count and inflammatory markers), and potentially a swab for sexually transmitted infections (STIs) are crucial to identify the presence of PID. Depending on the results, further imaging, such as ultrasound or CT scan, might be necessary.
If the diagnosis is confirmed, a treatment plan will be implemented that likely includes intravenous antibiotics to address the infection, often administered in a hospital setting.
Additional treatments may include pain management and supportive care. Patient education on sexual health, contraception, and the importance of follow-up appointments is vital.
Factors Influencing Severity
Several factors can influence the severity of PID in Sarah’s case. Her history of multiple sexual partners increases her risk of acquiring STIs, a significant contributing factor to PID. Consistent use of contraception and preventive measures could potentially have lessened the severity of the infection. Her response to antibiotic treatment and overall health status also play a crucial role.
Importance of Early Detection and Treatment
Early detection and treatment of PID are critical for preventing complications. If left untreated, PID can lead to serious long-term consequences, including infertility, chronic pelvic pain, and ectopic pregnancies. In Sarah’s case, prompt diagnosis and treatment can prevent these complications and maintain her reproductive health. The promptness of her seeking medical attention and the thoroughness of the diagnostic process will greatly influence the outcome.
Illustrative Images (Hypothetical)
Understanding Pelvic Inflammatory Disease (PID) often benefits from visual aids. These hypothetical illustrations can help visualize the complexities of the condition, from the initial infection to potential long-term consequences. They are not intended to be medical diagnoses, but rather educational tools.
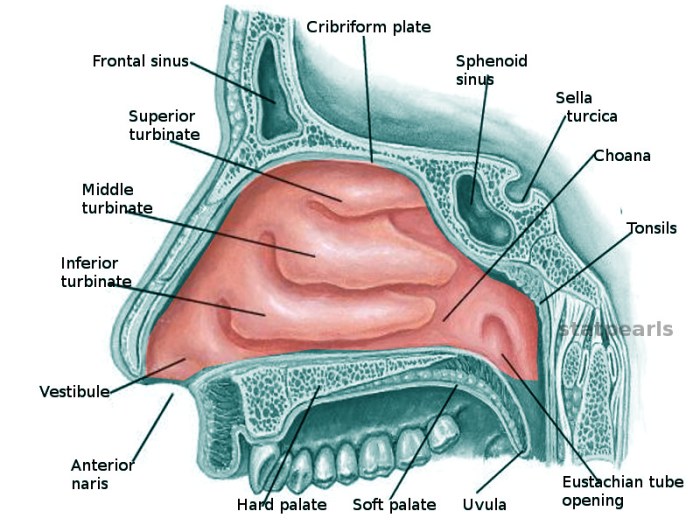
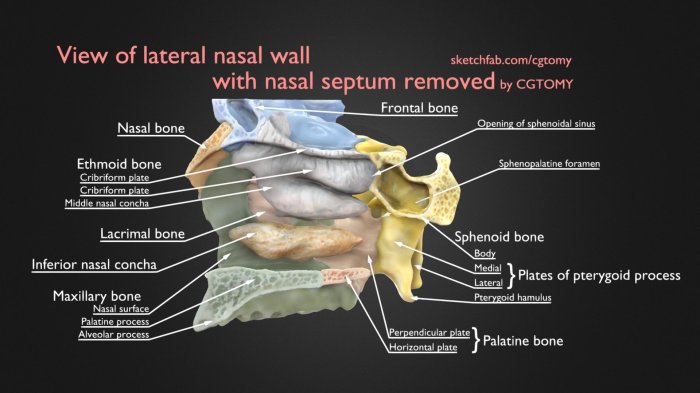
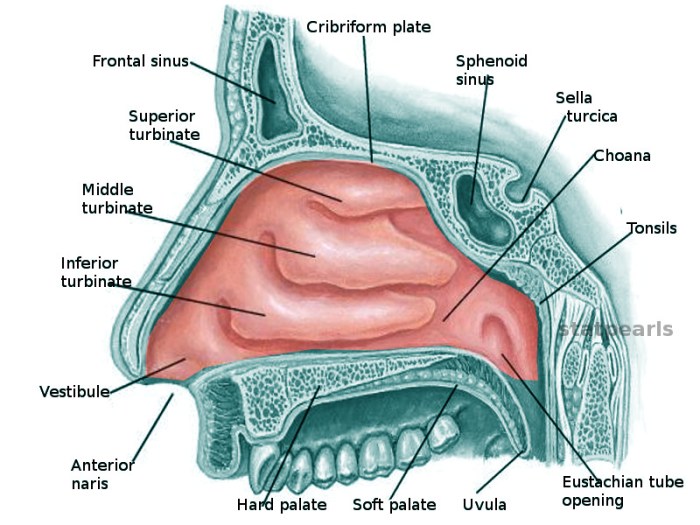
Reproductive Organs Affected by PID
This illustration shows a healthy female reproductive system, highlighting the uterus, fallopian tubes, and ovaries. A separate, overlayed image would indicate areas potentially affected by PID. This would include redness, swelling, and possible pus or fluid accumulation in the affected fallopian tubes, a key characteristic of PID. The illustration would also clearly distinguish between the normal, healthy structures and those exhibiting signs of inflammation.
Inflammatory Response in the Pelvic Region
A detailed illustration of the pelvic region would visually represent the inflammatory response. This would include a magnification of the affected fallopian tubes, showcasing the infiltration of immune cells and the release of inflammatory mediators. The illustration would depict the increased blood flow and swelling in the inflamed tissues. Color gradients could be used to visually represent the severity of the inflammation in different areas.
Spread of Infection in PID
This illustration would demonstrate the potential spread of infection in PID. It would start with the initial infection in the cervix or vagina, showing how it can ascend through the fallopian tubes. The illustration could then showcase the infection potentially spreading to the ovaries, uterus, or surrounding tissues. Arrows or color-coded zones could clearly mark the progression of the infection, emphasizing the importance of early diagnosis and treatment to prevent further spread.
Antibiotics Used in Treating PID
This illustration would visually display the various types of antibiotics commonly used to treat PID. It would include a diagram or table that lists different antibiotic classes (e.g., penicillins, cephalosporins, and metronidazole). Each class would be represented by a distinct color or shape. The illustration would also indicate the specific mode of action of each antibiotic, perhaps using simple icons to represent bacterial targets.
A legend would explain the different classes of antibiotics and their mechanism of action in combating the infection.
Closure
In conclusion, pelvic inflammatory disease (PID) requires careful attention to its symptoms, risk factors, and treatment options. Early detection and prompt treatment are vital to minimize complications and maintain reproductive health. This overview provides a foundational understanding of PID, empowering individuals to take proactive steps towards prevention and seek appropriate medical care when needed. Remember, knowledge is the first step toward managing and overcoming this condition.